When the body’s defense systems sacrifice the long run in favor of short run wins
Even after we have overcome a viral disease, our immune system is working hard to produce antibodies that give us protection against further exposure. But what happens if while we are recovering from the flu, or God forbid from the corona, we are exposed to another infection – let’s say salmonella from the chicken soup we ordered in delivery? In a new study published today in the scientific journal Immunity, Weizmann Institute of Science scientists have shown that the immune system has a sophisticated way of setting priorities in the event of various infections occurring one after the other, and that it may “sacrifice” immunity in the long run in favor of short-term gains. Understanding these priorities may help develop new therapies for autoimmune diseases.
Our immune system has two arms: the innate system and the acquired system. The innate system – the body’s first line of defense – goes into action when it senses the invasion of viruses, bacteria or other pathogens, and quickly neutralizes them through cells and biological substances that give the body a wide protective sheet. For the acquired system, however, it sometimes takes a few days to deploy its troops – dedicated cells and antibodies adapted to the various invaders with miraculous accuracy; These antibodies stay in the body for months and even years and give it long-term protection.
In other words, each of the systems occupies the center of the stage at different stages of dealing with the disease. But what happens when two different infections enter the body in close proximity, one after the other, and both arms are forced to be called to the flag at the same time? A research group led by Prof. Ziv Shulman of the Institute’s Immunology Department aims to find out how the immune system will deal with a situation where the innate system rolls up its sleeves to fight a new invader, while the acquired one produces antibodies against the previous invader. In a study led by research student Adi Biram, the scientists found that the overlap in the systems’ activity produced a collision: when mice recovering from the flu were infected with salmonella – dealing with the bacterial infection disrupted antibody production to the virus. That is, under a life-threatening threat, the immune system stops the mechanisms necessary for long-term protection and concentrates on the immediate danger.
The scientists found that the bacterial infection did not directly lead to the cessation of antibody production. When the salmonella penetrated the mice’s lymph nodes, an “alarm bell” was activated that resounded throughout the body and mobilized cells of the innate system located in the bone marrow called monocytes. These cells flooded the lymph nodes in an attempt to land a blow on the salmonella, thereby changing their environment: the antibacterial chemicals secreted by the cells led to conditions of oxygen deprivation.
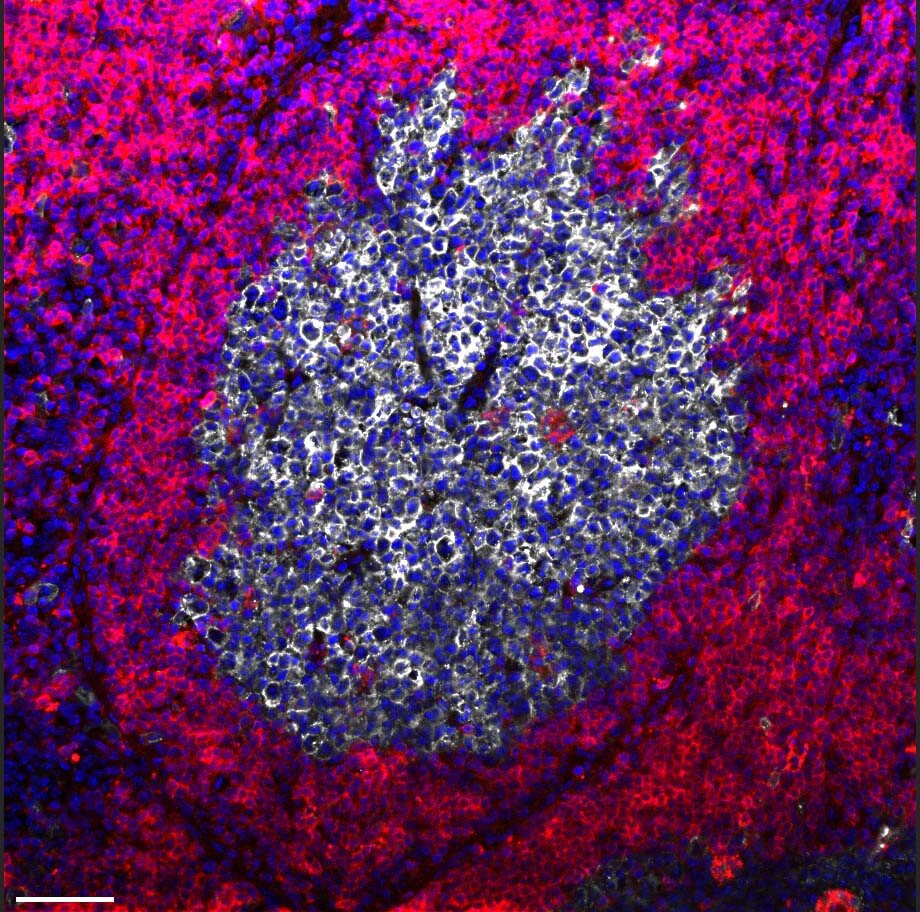
Immune system cells often know how to adapt to this type of environmental change and change their metabolism so that they are not dependent on oxygen for energy production – but the researchers found that there is a certain subtype of B cells for which oxygen deficiency becomes fatal. These cells play a key role in the action of the acquired system: they are the ones that produce the antibodies that are best suited for invaders within microscopic structures in the lymph nodes called “germinal centers”. These cells do not change their metabolism in response to oxygen deficiency, and as a result they suffocate and die. In the absence of these cells, the production of antibodies necessary for long-term protection against the influenza virus has ceased.
“When you have to fight life-threatening bacteria, you don’t mess with long-term protection,” explains Prof. Shulman. “Overcoming salmonella gets priority because it’s a matter of survival.”
Beyond a better understanding of the functioning of the immune system, the new findings may help us help the body’s defense systems. For example, it is known that in order to increase the effectiveness of certain vaccines currently given, it is customary to add to them proteins derived from bacteria; Judging by the new findings, it is possible that this practice may harm the purpose for which the vaccine was given: the production of antibodies. In addition, if the results of the study are also demonstrated in humans, they may mark a new therapeutic direction in autoimmune diseases. In diseases such as rheumatoid arthritis or lupus, improper production of antibodies causes the immune system to act against the body itself. Possible treatments may raise the monocytes from bone marrow, thus leading to the cessation of harmful antibody production.
Jinging Liu, Dr. Hadas Hatzroni, Dr. Natalia Davidson, Dr. Dominic Schmidel, Dr. Iman Khatib-Masalha, Montser Haddad, Dr. Amelia Granov, Prof. Zvi Lapidot and Prof. ‘Stefan Jung from the Institute’s Immunology Department; Sasha Lavon, Dotan Hoffman and Dr. Roi Avraham from the Institute’s Biological Control Department; Dr. Tomer Meir Selma from the Department of Life Sciences Infrastructure Research; Dr. Nili Dzorla from the Department of Chemical Research Infrastructures; Paula Abu Kerem from the Department of Biomolecular Sciences; And Prof. Mark Berk from the University of Gothenburg in Sweden.
More on the subject on the Knowledge website:
