Montreal, 2025-06-20 15:46:00 – A Montreal researcher recently obtained a major $ 1.2 million health research institutes from Canada to better understand glioblastoma, a notably aggressive and lethal form of brain cancer.
Unraveling the Brain’s Immune System
A new grant aims to decode glioblastoma’s resistance to treatment and find new immunotherapy approaches.
- Researchers are mapping the brain’s immune surroundings in glioblastoma.
- They are targeting myeloid cells that aid tumor growth and treatment resistance.
- The study will investigate the impact of surgery on tumor progression and relapse.
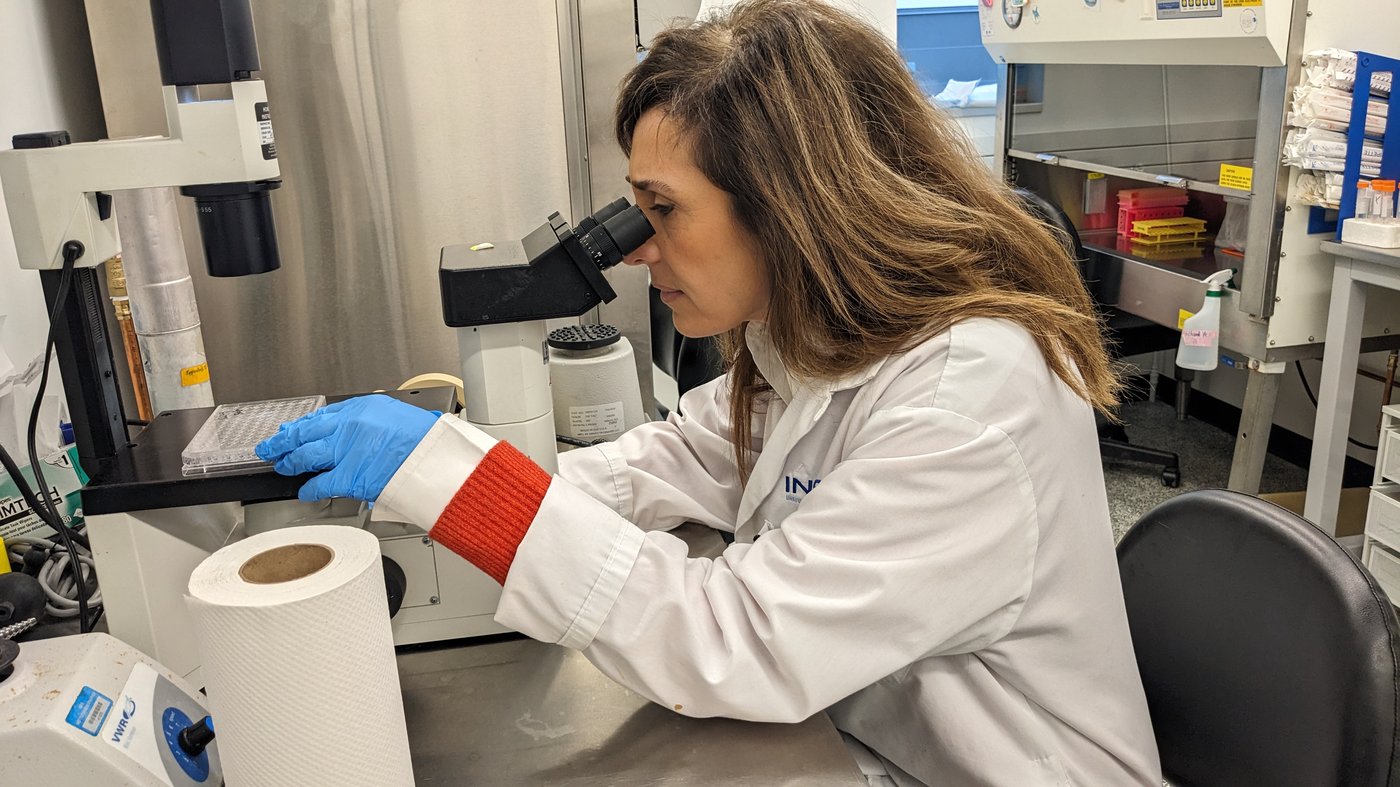
Professor Maya Saleh, from the Armand-Frappier Health Biotechnology Center of the National Institute for Scientific Research, and her team are on a mission to understand glioblastoma, a devastating form of brain cancer. they aim to map the brain’s immune environment, focusing on myeloid cells that contribute to tumor growth, which is critical because the average survival time after diagnosis is barely a year.
Glioblastoma: Key Facts
- most common malignant primary brain tumor in adults.
- Characterized by rapid growth and aggressive spread.
- median survival is only 12-15 months with current treatments.
“Despite the initial promise that the immune system could defend us and eliminate cancers if we inject these immunotherapy in patients,we see that the Pan-Cancer response rate is less than 20 %,” said Professor Saleh. The standard treatments for glioblastoma haven’t changed much in 40 years, and the tumor returns in over 90% of cases.
The Role of Myeloid Cells
The researchers are keen to understand why immunotherapy, which primarily uses T lymphocytes, has been ineffective against glioblastoma. T lymphocytes are not very present in the brain. Instead, monocytes, which can promote tumor growth, are prevalent. Professor Saleh’s work suggests surgery could paradoxically stimulate monocytes.
Myeloid Cells: A Double-Edged Sword
Myeloid cells,including monocytes,are part of the immune system but can be co-opted by tumors to promote growth and suppress anti-tumor immunity.
“The first objective (of the grant) is to understand, in fact, the impact of the surgical procedure on tumor progression and relapse,” said Professor Saleh. The surgical procedure may trigger inflammation, contributing to tumor relapse.
“So what interests us are the resistance mechanisms. We work on immunological mechanisms, what are the combinations of new immunotherapy that can be added.”
Mapping the Brain’s Battlefield
The brain is a “very special” organ, said the researcher, and immunotherapy works ther “at 0 %”. They aim to identify signals that differentiate cells and where they can intervene.
“When they arrive at the brain, (some) monocytes become immunosuppressive,” said Professor Saleh. “The idea is that we must understand what are the signals that will differentiate the cells (…) and where we could intervene.”
The team is collaborating with doctors Sami Obaid and Romain Cayrol of the University of Montreal hospital, analyzing biopsies taken from patients.They also use mass spectrometry to study the tumor environment’s glucose, lipids, and other compounds.Advanced technologies like space biology, which INRS is the only establishment in Canada to own, are used to analyze the tissues.
Leveraging Artificial Intelligence
A biostatistician at INRS, Amadou Barry, is developing artificial intelligence algorithms to analyze the complex data from space biology. Artificial intelligence is key to understanding cancer and improving treatment. As a notable example, the team found that the tumor center’s cells run out of oxygen, consume glucose, and produce lactate as the tumor grows.
“Today, with artificial intelligence, we need to better understand the nature of cancer to better treat it,” said Professor Saleh. “And we have a hypothesis that lactate modifies the immune environment by making it more immunosuppressive,” said the researcher.
“There is still a lot to discover, but there is also a lot of progress,” concluded Professor Saleh.”I am optimistic that in a few years we will even have clinical (positive) clinical trials. “
Unlocking Glioblastoma Treatment: Promising New Avenues
Professor Saleh’s research into glioblastoma, the most common adn aggressive form of brain cancer, is crucial in the fight against this devastating disease [[1]]. The team’s focus on the brain’s immune surroundings, notably the role of myeloid cells, offers a promising new approach, building on the understanding that current treatments often fail due to the tumor’s ability to evade the immune system.Glioblastoma recurrence is a significant challenge, making it imperative to find innovative ways to prevent the tumor from returning.
The Challenge of Glioblastoma Recurrence
The high recurrence rate for glioblastoma remains a major hurdle in treatment. Traditional therapies, like surgery, radiation, and chemotherapy, often fail. Even when initially prosperous, the cancer frequently returns, sometimes in a more aggressive form [[1]].Professor Saleh’s work, highlighted in earlier sections, aims to address this, seeking to understand why current immunotherapies struggle and identifying new strategies to overcome these challenges.
Current Treatment approaches and Their Limitations
Standard treatments for glioblastoma, including surgery, radiation therapy, and chemotherapy, have limitations. While surgery aims to remove the tumor, it can be arduous to eliminate all cancerous cells. Radiation and chemotherapy can damage healthy brain tissue, leading to side effects, and the cancer cells often develop resistance. Immunotherapy, though promising, has had limited success due to the brain’s unique immune environment.
Emerging Immunotherapy Strategies
Several new immunotherapy approaches are being explored to improve glioblastoma treatment:
- CAR-T Cell Therapy: This involves modifying a patient’s T cells to recognize and attack cancer cells.Some clinical trials have shown promising results, with rapid regression of glioblastoma tumors [[3]].
- Checkpoint Inhibitors: these drugs work by releasing the “brakes” on the immune system, allowing T cells to attack cancer cells more effectively. Though, these have had limited success.
- Combination Therapies: Researchers are exploring combinations of different immunotherapies or combining them with other treatments, such as chemotherapy or targeted therapies.
The Role of Clinical Trials
Clinical trials play a vital role in advancing glioblastoma treatment. These trials test new therapies, assess their safety and effectiveness, and provide hope for patients. Participating in a clinical trial can be an option for patients seeking advanced treatment options. Research like Professor Saleh’s work helps to inform and improve these clinical trials.
Benefits of New Approaches
The development of novel approaches to glioblastoma treatment has several potential benefits:
- Improved Survival Rates: New therapies show promise in increasing the lifespan of patients diagnosed with glioblastoma.
- Enhanced Quality of Life: Improved treatments can lead to fewer side effects and an improved quality of life.
- Reduced Recurrence: Strategies to prevent recurrence could significantly extend disease-free survival.
It is significant to note that early detection and prompt treatment are critical for the best outcomes in glioblastoma.
Looking Ahead
Professor Saleh’s research and other ongoing studies are crucial for improving glioblastoma treatment. A key goal is developing more effective and targeted therapies, wich can overcome treatment resistance and prevent recurrence. Understanding the brain’s immune environment and the mechanisms by which tumors evade the immune system is basic to these advances. The future holds promise for better outcomes and improved quality of life for those affected by this devastating disease.
Table of Contents