“`html
Will Tiny Lab-Grown Organs Replace Animal Testing? The Future of Medicine is Here
Table of Contents
- Will Tiny Lab-Grown Organs Replace Animal Testing? The Future of Medicine is Here
- Organ-on-a-Chip Technology: Revolutionizing Drug Progress and Beyond – an Expert Interview
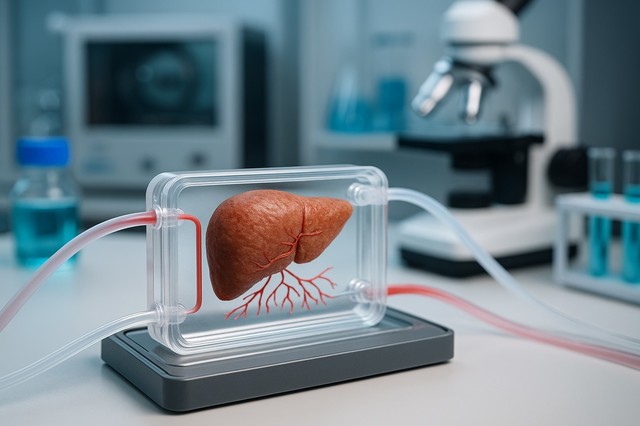
imagine a world where new drugs are tested not on animals or humans, but on miniature, lab-grown organs. Sounds like science fiction? Think again. Organ-on-a-chip (OOC) technology is rapidly advancing, promising to transform biomedical research and drug development as we certainly know it.
The Promise of Organs-on-Chips: A New Era in Medical Research
Organs-on-chips, also known as microphysiological systems, are engineered miniature tissues grown inside microfluidic chips [[2]]. These chips mimic the complex structures and functions of living human organs [[1]], offering a more accurate and consistent way to study diseases and test new treatments.
But there’s been a catch: these mini-organs lacked a crucial component – functional blood vessels. Now, a breakthrough from researchers at the Vienna Technical University (Tu Wien, Austria) and Keio University (japan) is poised to change everything.
Cracking the Code: Creating Realistic Blood Vessels in Mini-Organs
The key innovation? A novel method using ultra-short laser pulses to rapidly and reproducibly create artificial blood vessels within these miniature organ models. These aren’t just any blood vessels; lab tests confirm thay behave remarkably like their natural counterparts.
The Laser Precision Advantage
The team uses state-of-the-art laser technology, employing extremely short laser impulses (femtoseconds) to create precise, three-dimensional structures directly within a gelatinous material called hydrogel. “We can create channels spaced in only one hundred micrometers. This is essential if we want to reply the natural density of the vessels in a specific organ,” said Prof. Aleksandr Ovsianikov, head of the 3D Printing & Biofabrication department, from TU Wien.
Overcoming the Geometry Challenge
Previously, controlling the shape and size of these microvascular networks was a major hurdle. Some methods relied on “self-organization,” leading to inconsistent results. The new laser-based approach offers unprecedented control and reproducibility, essential for reliable medical research.
Why This Matters: The Impact on Drug Development and Personalized Medicine
So, why is this breakthrough so notable? Here’s how it could reshape the future of medicine:
- Faster, More Accurate drug Testing: imagine testing a new drug’s effect on a human liver, kidney, or heart *before* it ever reaches clinical trials. oocs with functional blood vessels make this a reality, possibly saving time, money, and lives.
- Reduced Reliance on Animal Testing: The ethical implications are huge. OOC technology offers a viable option to animal testing,aligning with growing public and regulatory pressure to reduce animal use in research.
- Personalized Medicine Revolution: In the future, doctors could use OOCs created from a patient’s own cells to determine the most effective treatment for their specific condition. This personalized approach could dramatically improve treatment outcomes.
The liver chip: A Major Success Story
One of the most promising applications is in liver research. Replicating the liver’s complex microvascularization has been a long-standing challenge. “Using this approach, we managed to vascularize a liver model,” explained Prof. Ovsianikov. This breakthrough allows researchers to study liver diseases,drug metabolism,and toxicity with unprecedented accuracy.
Challenges and Future Directions
While the progress is remarkable, challenges remain. Scaling up production of oocs for widespread use is a key hurdle. Ensuring the long-term stability and functionality of these artificial organs is also crucial.
Pros and Cons of Organ-on-a-Chip Technology
| Pros | Cons |
|---|---|
| Reduces animal testing | high initial development costs |
| More accurate and relevant than animal models | Scalability challenges for mass production |