Flu Deaths Among US Children Reach Alarming Levels: A Deep dive into the crisis adn What Lies Ahead
Table of Contents
- Flu Deaths Among US Children Reach Alarming Levels: A Deep dive into the crisis adn What Lies Ahead
- The Grim Reality: Pediatric Flu Deaths Soar
- Why Are Children So Vulnerable This Year?
- Beyond Vaccination: Underlying Health Conditions and Flu Strains
- The Impact on Adults: A “Highly Serious” Season
- Looking Ahead: What Can Be Done?
- The role of Public Health Messaging
- The Economic Impact of Flu
- The Ethical Considerations
- FAQ: Your Burning Questions Answered
- Pros and cons of Flu Vaccination
- Expert Quotes and Testimonies
- The future of Flu Prevention
- Flu Crisis: Understanding the Alarming Rise in Pediatric Flu Deaths – An Expert Interview
Are we facing a silent epidemic? The latest CDC report reveals a chilling reality: the number of American children succumbing to the flu this season has reached a peak unseen since the 2009 H1N1 pandemic. With 216 pediatric deaths already recorded, exceeding last year’s 207, the question isn’t just *what* happened, but *what’s next*?
The Grim Reality: Pediatric Flu Deaths Soar
The numbers paint a stark picture. This flu season has been particularly brutal for children, marking the deadliest period in 15 years. While the flu season is showing signs of slowing down, experts warn that the final toll could be even higher as data continues to be compiled. This isn’t just a statistic; it represents real families grappling with unimaginable loss.
Dr. Sean O’Leary, a pediatric infectious disease specialist at the University of Colorado and member of the American Academy of Pediatrics, emphasizes the underestimation of the current figures. “The current figure is most certainly underestimated and will increase as the season ends and all the data will be compiled,” he stated, highlighting the urgent need for proactive measures.
Why Are Children So Vulnerable This Year?
several factors contribute to this alarming trend. One of the most critically important is a concerning drop in childhood vaccination rates. in just five years,the vaccination rate has plummeted from approximately 64% to a mere 49%. This decline leaves a ample portion of the pediatric population susceptible to severe flu complications.
The Vaccination Rate Plunge: A Multifaceted Problem
The decline in vaccination rates isn’t a simple issue. It’s a complex interplay of factors, including:
- Misinformation and Vaccine Hesitancy: The spread of online disinformation, fueled by controversies surrounding COVID-19 vaccines, has eroded public trust in vaccines in general.
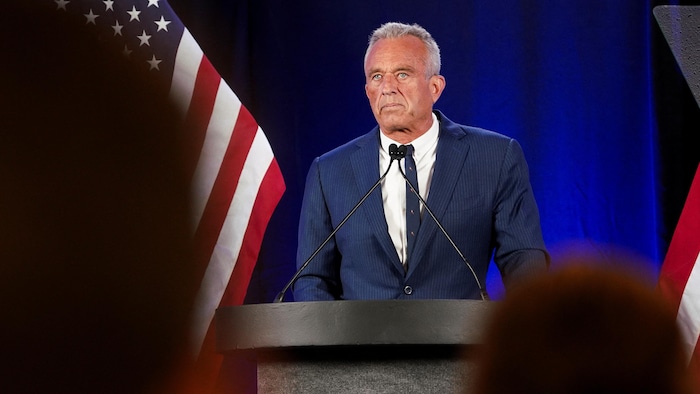
- Political Influence: Figures like Robert F. Kennedy Jr., now a prominent political figure, have amplified anti-vaccine sentiments, further contributing to vaccine hesitancy.
- Healthcare Access Challenges: Staff shortages in pediatric practices and limited vaccination availability outside of regular office hours create barriers to access.
- Pharmacy Limitations: While pharmacies are increasingly offering vaccinations, many do not administer them to young children, leaving a gap in accessibility.
Expert Tip: Check with your pediatrician or local health department to find convenient vaccination clinics and times. Many offer evening and weekend appointments to accommodate busy schedules.
Beyond Vaccination: Underlying Health Conditions and Flu Strains
While vaccination plays a crucial role, other factors also influence the severity of flu cases. The CDC reports that among hospitalized adults, nearly 95% had at least one underlying health condition. In contrast, only 53% of hospitalized children had pre-existing conditions like asthma or obesity. This suggests that even healthy children are at risk of severe flu complications.
The Role of Flu Strain Diversity
This season has also been marked by a greater diversity of circulating influenza strains, particularly two type A viruses: H1N1 and H3N2. While early data suggests that flu vaccines remain effective in preventing deaths and hospitalizations, the increased diversity of strains poses a challenge to public health efforts.
Did you know? The flu virus is constantly mutating, which is why a new flu vaccine is developed each year to target the most prevalent strains.
The Impact on Adults: A “Highly Serious” Season
while the focus is on pediatric deaths, the flu season has also been severe for adults. The CDC characterizes it as “highly serious,” with approximately 47 million cases, 610,000 hospitalizations, and 26,000 deaths reported across the United States. This underscores the widespread impact of the flu and the importance of vaccination for all age groups.
Looking Ahead: What Can Be Done?
The current situation demands immediate and sustained action. Here’s what needs to happen:
Boosting Vaccination Rates: A National Priority
Increasing vaccination rates is paramount. This requires a multi-pronged approach:
- Combating Misinformation: Public health campaigns must actively counter online disinformation and promote accurate information about vaccine safety and efficacy.
- Addressing Vaccine Hesitancy: Healthcare providers need to engage in open and honest conversations with parents,addressing their concerns and providing evidence-based information.
- Improving Access: Expanding vaccination access through school-based clinics, mobile vaccination units, and partnerships with pharmacies is crucial.
- Policy Interventions: Exploring policy options such as mandatory vaccination for school attendance (with medical exemptions) could be considered.
Strengthening Healthcare Infrastructure
Addressing staff shortages in pediatric practices and ensuring adequate resources for flu testing and treatment are essential. This includes:
- Investing in Healthcare Workforce: Providing incentives for healthcare professionals to specialize in pediatrics and infectious diseases.
- Expanding Telehealth Services: Utilizing telehealth to provide remote consultations and monitor patients with flu symptoms.
- Ensuring Adequate Supplies: Maintaining sufficient stockpiles of antiviral medications and diagnostic tests.
Enhanced Surveillance and Research
Continuous monitoring of circulating flu strains and research into more effective vaccines are critical for long-term preparedness. This includes:
- Genomic Sequencing: Tracking the evolution of flu viruses through genomic sequencing to identify emerging strains.
- Developing Universal Flu Vaccines: Investing in research to develop universal flu vaccines that provide broader and longer-lasting protection.
- Improving Diagnostic Tools: Developing rapid and accurate diagnostic tests to facilitate timely treatment.
The role of Public Health Messaging
Clear and consistent public health messaging is vital. The CDC and other health organizations must communicate effectively with the public about the importance of vaccination, hygiene practices, and early treatment. This includes:
- Targeted Campaigns: Developing targeted campaigns for specific populations, such as parents of young children and individuals with underlying health conditions.
- Utilizing Social Media: Leveraging social media platforms to disseminate accurate information and counter misinformation.
- Community Engagement: Partnering with community leaders and organizations to promote health literacy and build trust.
The Economic Impact of Flu
The flu has a significant economic impact, resulting in lost productivity, healthcare costs, and absenteeism from school and work. Investing in flu prevention and treatment is not only a public health imperative but also an economic one.
Quantifying the Costs
The CDC estimates that the flu costs the United States billions of dollars each year. This includes:
- Direct Medical Costs: Doctor visits, hospitalizations, and medications.
- Indirect Costs: Lost wages, reduced productivity, and absenteeism.
- Public Health Expenditures: Vaccination programs, surveillance activities, and public health campaigns.
Fast Fact: The flu can lead to complications such as pneumonia, bronchitis, and sinus infections, further increasing healthcare costs.
The Ethical Considerations
The flu raises ethical considerations related to vaccine mandates, resource allocation, and individual autonomy. Balancing the rights of individuals with the need to protect public health is a complex challenge.
Ethical frameworks can guide decision-making in the context of the flu. This includes:
- Utilitarianism: Maximizing the overall benefit for the greatest number of people.
- Justice: Ensuring equitable access to vaccines and treatment.
- Respect for Autonomy: Respecting individuals’ right to make informed decisions about their health.
FAQ: Your Burning Questions Answered
Here are some frequently asked questions about the flu and its impact:
- What are the symptoms of the flu?
-
Common symptoms include fever, cough, sore throat, body aches, headache, fatigue, and sometimes vomiting and diarrhea.
- How is the flu spread?
-
The flu is spread through respiratory droplets produced when an infected person coughs, sneezes, or talks.
- How can I protect myself from the flu?
-
Get vaccinated annually, practice good hygiene (wash your hands frequently), avoid touching your face, and stay home if you are sick.
- Is the flu vaccine safe?
-
Yes, the flu vaccine is safe and effective. Serious side effects are rare.
- What should I do if I think I have the flu?
-
Stay home, rest, drink plenty of fluids, and contact your doctor if your symptoms are severe or if you have underlying health conditions.
Pros and cons of Flu Vaccination
Flu vaccination is a widely recommended preventive measure, but it’s essential to consider both its advantages and disadvantages.
Pros
- Reduced Risk of Infection: vaccination substantially lowers the likelihood of contracting the flu.
- Milder Symptoms: even if you get the flu after vaccination, symptoms are often less severe.
- Prevention of Complications: Vaccination reduces the risk of serious complications like pneumonia and hospitalization.
- Community Protection: Higher vaccination rates protect vulnerable populations who cannot be vaccinated.
Cons
- Possible Side Effects: Some people experience mild side effects like soreness, fever, or body aches.
- not 100% Effective: The flu vaccine is not always fully effective, especially if the circulating strains are different from those targeted by the vaccine.
- Annual Vaccination Required: As the flu virus mutates, a new vaccine is needed each year.
- Allergic Reactions: Rare but possible allergic reactions to vaccine components.
Expert Quotes and Testimonies
“Vaccination is the best way to protect yourself and your family from the flu,” says Dr.Anthony Fauci, former director of the National Institute of Allergy and Infectious Diseases. “It’s a safe and effective way to reduce your risk of getting sick and spreading the virus to others.”
“We need to do a better job of educating the public about the importance of vaccination,” says Dr. Rochelle Walensky, former director of the CDC. “Misinformation and vaccine hesitancy are putting people at risk.”
The future of Flu Prevention
The current flu season serves as a stark reminder of the ongoing threat posed by influenza. By investing in research, strengthening healthcare infrastructure, and promoting vaccination, we can better protect ourselves and our communities from future outbreaks.
The fight against the flu is a marathon, not a sprint.It requires sustained effort, collaboration, and a commitment to evidence-based public health practices. The lives of our children and the health of our nation depend on it.
Call to Action: Share this article with your friends and family to raise awareness about the importance of flu prevention. Talk to your doctor about getting vaccinated and encourage others to do the same. Together, we can protect our communities from the flu.
Flu Crisis: Understanding the Alarming Rise in Pediatric Flu Deaths – An Expert Interview
Time.news: Welcome, Dr. Vivian Holloway. Thanks for joining us today to discuss the concerning rise in pediatric flu deaths this season.The numbers are alarming. The CDC’s latest report paints a grim picture, with pediatric flu deaths exceeding those of recent years. Are we truly facing a crisis?
Dr. Holloway: Thank you for having me. Yes, the situation is undoubtedly concerning. The increase in pediatric flu deaths this season, reaching levels not seen as the 2009 H1N1 pandemic, is a serious public health issue that demands our immediate attention. While we’re seeing the tail end of the flu season, the data suggests the final numbers may still rise as facts is compiled.
Time.news: What factors are contributing to this spike in severe flu cases among children?
Dr. Holloway: Several factors are at play. The most important is the concerning drop in childhood vaccination rates. Over the past five years, we’ve witnessed a substantial decline, from approximately 64% to around 49%. This leaves a significant segment of the pediatric population vulnerable to severe flu complications.
Time.news: Why are flu vaccination rates plummeting? What’s behind this trend?