The Long Shadow of Breast Cancer: Understanding Late Recurrence and Dormant Disease
Table of Contents
Despite advancements in treatment, breast cancer can return years, even decades, after initial remission. New research is increasingly focused on understanding the mechanisms behind this late recurrence, particularly the role of dormant tumor cells and minimal residual disease (MRD). This article synthesizes findings from recent studies to illuminate the challenges and emerging strategies in combating this persistent threat.
The Persistence of Recurrence: A Decades-Long Risk
Historically, breast cancer recurrence was largely considered within the first five years post-treatment. However, studies reveal a significant risk extending far beyond this timeframe. A study by Pedersen et al. (2022) demonstrated that recurrence can occur 10–32 years after primary diagnosis, highlighting the need for long-term surveillance and a deeper understanding of the biological processes at play. The International Breast Cancer Study Group trials, spanning 24 years of follow-up (Colleoni et al., 2016), further underscore this protracted risk, showing that the hazard rate of recurrence, while decreasing over time, remains non-zero for many years.
A key factor in late recurrence is the phenomenon of cancer cell dormancy. Dormant tumor cells are cancer cells that remain inactive, evading detection and treatment, only to reawaken and initiate metastatic growth years later. Researchers are increasingly recognizing that these cells aren’t simply quiescent, but actively adapting to their environment. As Dalla et al. (2023) explain, dormancy is a complex state involving intricate interactions between cancer cells and their microenvironment.
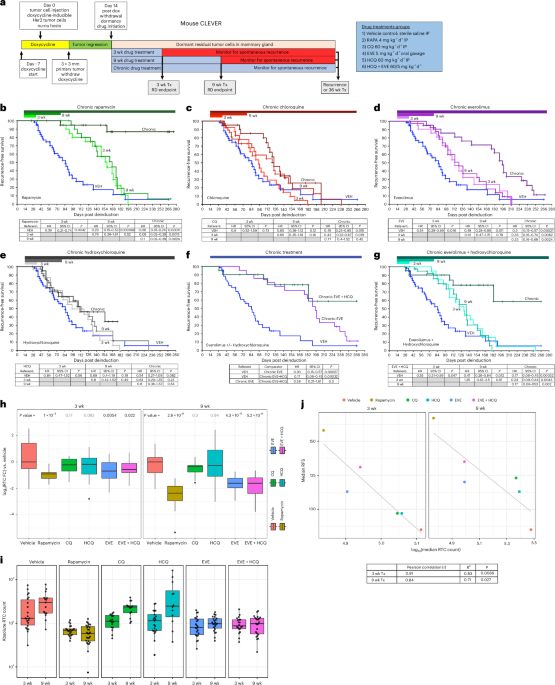
The mechanisms driving dormancy are multifaceted. Studies have identified roles for autophagy – a cellular “self-eating” process – in promoting the survival of dormant cells (Vera-Ramirez et al., 2018; Dwyer et al., 2024). Conversely, inhibiting autophagy can sometimes trigger these cells to emerge from dormancy, highlighting the delicate balance involved. Other factors, such as the transcriptional repressor Snail (Moody et al., 2005), and signaling pathways involving c-MYC (D’Cruz et al., 2001) have also been implicated in establishing and maintaining dormancy.
Disseminated Tumor Cells: Seeds of Future Recurrence
The spread of cancer cells beyond the primary tumor – known as disseminated tumor cells (DTCs) – is a critical step in the development of metastasis and late recurrence. DTCs can travel through the bloodstream and lodge in distant organs, where they may remain dormant for years. Research by Braun et al. (2005) demonstrated the presence of bone marrow micrometastasis in breast cancer patients, suggesting the bone marrow as a common site for DTCs.
The prognostic significance of DTCs is well-established. Studies by Hall et al. (2012) and Mathiesen et al. (2012) showed that the persistence of DTCs after neoadjuvant therapy is a strong predictor of poor survival. International pooled analyses (Hartkopf et al., 2021) confirm the prognostic value of DTCs, even in early-stage breast cancer. However, detecting these cells remains a challenge, and standardized methods for their detection and quantification are continually being refined (Fehm et al., 2006; Tolaney et al., 2021).
Emerging Therapeutic Strategies: Targeting MRD
The growing understanding of dormancy and MRD is driving the development of new therapeutic strategies aimed at preventing late recurrence. Therapeutic targeting of minimal residual disease is a promising approach, focusing on eliminating these remaining cancer cells before they can reawaken and form metastases (Cescon et al., 2021).
Several avenues are being explored. Circulating tumor DNA (ctDNA) analysis, which detects cancer-specific mutations in the bloodstream, is emerging as a powerful tool for identifying MRD and monitoring treatment response (Coombes et al., 2019; Garcia-Murillas et al., 2015). Clinical trials are investigating the use of ctDNA-guided therapies to personalize treatment and prevent recurrence.
Furthermore, research is focusing on disrupting the mechanisms that support dormancy. For example, studies have shown that targeting the Notch signaling pathway can prevent the recurrence of dormant tumor cells following HER2/neu-targeted therapy (Abravanel et al., 2015). The role of B3GALT6 in promoting dormant cell survival via FGF signaling is also being investigated as a potential therapeutic target (Sreekumar et al., 2024). The impact of metabolic factors, such as the role of autophagy, is also under scrutiny, with ongoing research exploring the potential of autophagy inhibitors.
The Influence of Lifestyle and Comorbidities
Beyond the biological mechanisms, lifestyle factors and comorbidities are increasingly recognized as playing a role in recurrence risk. Obesity, for instance, has been shown to impact both recurrence and MRD (Ecker et al., 2019). The interplay between obesity and menopause in promoting escape from tumor dormancy is a particularly concerning area of research (Roy et al., 2022).
Future Directions and Clinical Implications
The fight against breast cancer recurrence is evolving. Future research will likely focus on refining MRD detection methods, identifying novel therapeutic targets within dormant cells, and developing personalized treatment strategies based on individual risk profiles. The results of ongoing clinical trials, such as the phase III trial evaluating endocrine therapy plus everolimus (Chavez-MacGregor et al., 2024), will provide valuable insights into the effectiveness of new approaches. Ultimately, a comprehensive understanding of the complex interplay between tumor biology, the microenvironment, and patient-specific factors will be crucial for preventing the long shadow of breast cancer recurrence.