Rare Blood Disorder Linked to Dupilumab Treatment for Eustachian Tube Dysfunction
A patient experiencing treatment with dupilumab for Eustachian tube dysfunction developed a rare and severe blood disorder, acute severe immune thrombocytopenia (ITP), according to a recently published case report. The findings highlight the potential for unexpected adverse effects even when medications are used “off-label” – for conditions beyond their approved indications – and underscore the importance of vigilant monitoring.
Dupilumab, typically prescribed for conditions like eczema, asthma, and chronic rhinosinusitis with nasal polyps, works by blocking the signaling of interleukin-4 and interleukin-13, key proteins involved in inflammation. While generally considered safe, this case suggests a possible, though currently unconfirmed, link between the drug and a dangerous drop in platelet count.
Off-Label Use and Initial Symptoms
The case detailed in Cureus involves a patient who sought treatment for chronic Eustachian tube dysfunction, a condition causing blockage or malfunction of the tubes connecting the middle ear to the back of the throat. Standard treatments often prove ineffective, leading physicians to explore alternative therapies. In this instance, a physician opted to use dupilumab off-label, hoping to reduce inflammation contributing to the dysfunction.
Initial treatment appeared to show some improvement in the patient’s symptoms. However, approximately two months into the treatment regimen, the patient began experiencing symptoms indicative of a bleeding disorder, including petechiae – small, pinpoint-sized red spots on the skin – and mucosal bleeding.
Diagnosis and Treatment of Immune Thrombocytopenia
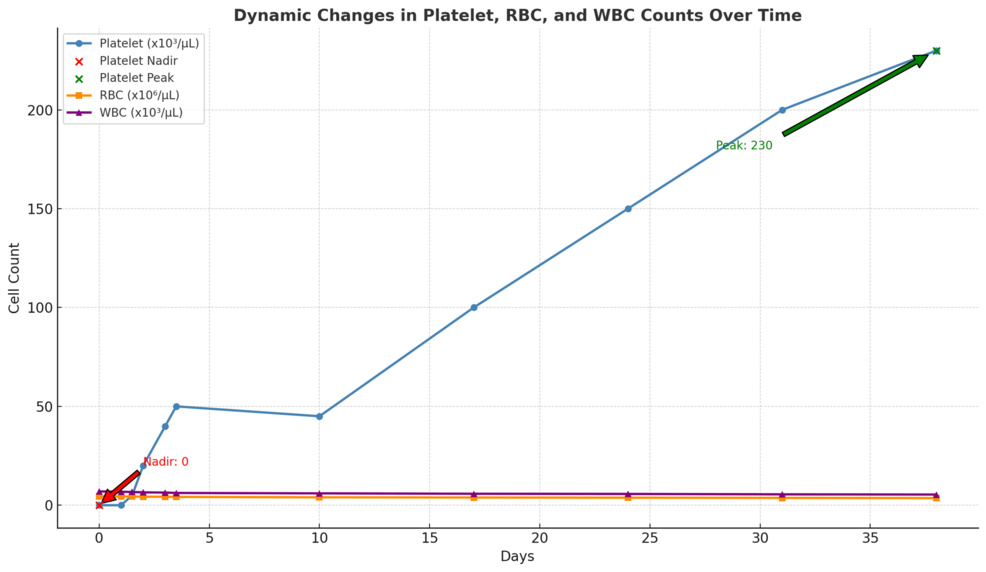
Further investigation revealed critically low platelet levels, leading to a diagnosis of acute severe immune thrombocytopenia (ITP). Platelets are essential for blood clotting, and a significant reduction can lead to serious, even life-threatening, bleeding. “The rapid onset and severity of the thrombocytopenia raised concerns about a potential drug-induced etiology,” the report stated.
The patient was immediately hospitalized and received treatment for the ITP, including high-dose corticosteroids and intravenous immunoglobulin (IVIG). These treatments aim to suppress the immune system and temporarily boost platelet counts. While the patient initially responded to treatment, the case report emphasizes the seriousness of the adverse event.
Implications and Future Research
This case report represents a single instance and does not establish a definitive causal relationship between dupilumab and acute severe immune thrombocytopenia. However, it serves as a crucial warning to healthcare professionals considering off-label use of the drug.
Several key points warrant further investigation:
- The potential for dupilumab to trigger autoimmune responses, specifically targeting platelets.
- The need for increased awareness among physicians regarding this potential adverse effect.
- The importance of baseline and regular monitoring of platelet counts in patients receiving dupilumab, particularly those using it for off-label indications.
“Further research, including larger observational studies and clinical trials, is needed to determine the true risk of ITP associated with dupilumab use,” one analyst noted. The report concludes that clinicians should carefully weigh the potential benefits and risks before prescribing dupilumab for conditions outside of its approved uses and remain vigilant for any signs of bleeding or thrombocytopenia.