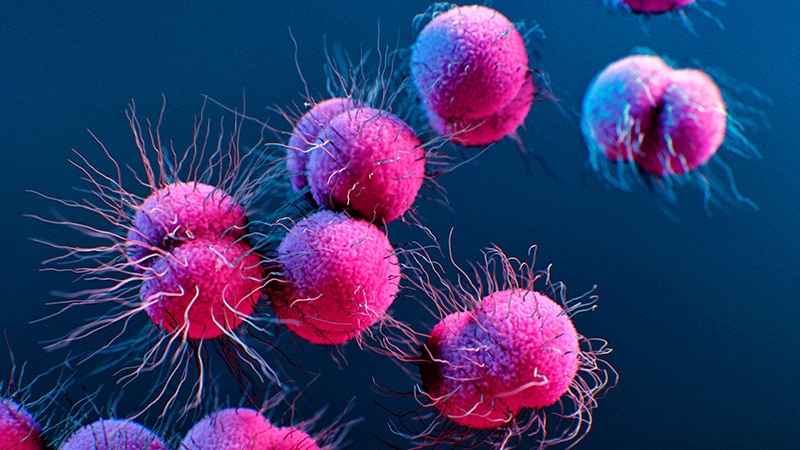
The Silent Epidemic: Are We Losing the Fight Against super Gonorrhea?
Imagine a world where a simple infection becomes a life-threatening crisis. That future may be closer than we think.While overall gonorrhea cases are down, a terrifying new threat is emerging: antibiotic-resistant strains, and they’re spreading faster than ever.
A Glimmer of Hope, Overshadowed by Resistance
the UK’s recent report offers a mixed bag. A 16% drop in gonorrhea diagnoses is certainly welcome news, particularly among young peopel. But this victory is threatened by the alarming rise of strains resistant to ceftriaxone, the go-to antibiotic for treatment.
Think of it like this: we’ve developed a powerful weapon against gonorrhea,but the bacteria are evolving,learning to deflect our attacks. What happens when our weapon becomes useless?
The Ceftriaxone Crisis: A Ticking Time Bomb
Ceftriaxone resistance is still relatively rare in the UK, but the trend is deeply concerning. The UKHSA reports that in the first five months of 2025, 14 cases of ceftriaxone-resistant gonorrhea have been identified, surpassing the 13 recorded in all of 2024.Six of those cases were extensively drug-resistant, meaning they shrugged off even second-line treatments. This isn’t just a UK problem; its a global one, with many resistant cases linked to travel from the Asia-Pacific region.
Why is this happening?
Overuse and misuse of antibiotics are the primary culprits. Just like with other superbugs, bacteria adapt and evolve to survive in the face of antibiotic pressure. This highlights the urgent need for responsible antibiotic stewardship.
expert Tip: Always complete the full course of antibiotics prescribed by your doctor,even if you start feeling better. Stopping early can contribute to antibiotic resistance.
STI Trends in England: A Broader Outlook
The UKHSA data paints a complex picture of sexual health trends:
- Total new STI diagnoses fell by 8.8%.
- Chlamydia cases decreased by 13%.
- Genital warts cases fell by 4.3% among 15- to 17-year-olds.
- Syphilis cases rose 4.6% overall.
- Genital herpes rose 3.5%.
These figures underscore the importance of comprehensive sexual health education and accessible testing.
The American Angle: What Does This Mean for the US?
While the UK data provides valuable insights, it’s crucial to consider the implications for the United States.The CDC has also been tracking rising rates of antibiotic-resistant gonorrhea. In 2020, the CDC reported a meaningful increase in resistance to azithromycin, another antibiotic commonly used to treat gonorrhea. This mirrors the UK’s ceftriaxone resistance concerns and highlights a global challenge.
Did you know? The CDC estimates that there are over 1.6 million new gonorrhea infections in the US each year, many of which go undiagnosed.
Testing: The First Line of Defence
Both UK and US health officials emphasize the critical role of regular STI testing. Dr. Hamish Mohammed of the UKHSA urges anyone who has had unprotected sex with new or casual partners to get tested at least annually, even without symptoms. Dr. Amanda Doyle of NHS England reinforces that STI testing is free and accessible.
In the US,Planned Parenthood and local health departments offer affordable and confidential STI testing services. Early detection is key to preventing the spread of infection and minimizing the risk of complications.
Vaccination: A New Weapon in the Arsenal
The UK’s launch of the world’s first gonorrhoea vaccination program is a game-changer. By repurposing the existing meningococcal B (4CMenB) vaccine, they aim to reduce gonorrhoea incidence by up to 40% in at-risk groups. This innovative approach could pave the way for similar vaccination programs in the US and other countries.
Quick Fact: Observational studies suggest the 4CMenB vaccine may offer cross-protection against gonorrhoea due to genetic similarities between the two bacteria.
The Future of Gonorrhea Treatment: A Call to Action
The rise of antibiotic-resistant gonorrhea demands a multi-pronged approach:
- Increased investment in research and advancement of new antibiotics.
- Enhanced surveillance and monitoring of antibiotic resistance patterns.
- Expanded access to comprehensive sexual health education and testing.
- Implementation of widespread vaccination programs.
- Promotion of responsible antibiotic use.
We must act now to prevent a future where gonorrhea becomes untreatable. The health of our communities depends on it.
Pros and Cons of the Gonorrhea Vaccine Program
Pros:
- Potential to considerably reduce gonorrhea incidence, especially in high-risk groups.
- Utilizes an existing vaccine, reducing development time and costs.
- May offer cross-protection against other related bacteria.
Cons:
- Vaccine effectiveness may vary depending on the strain of gonorrhea.
- Long-term impact on antibiotic resistance is still unknown.
- Potential for vaccine hesitancy among certain populations.
The Role of public Health Initiatives
Effective public health campaigns are crucial for raising awareness about STIs and promoting safe sexual practices. These initiatives should target high-risk populations and provide culturally sensitive information about prevention, testing, and treatment.
Call to Action: Share this article with your friends and family to help raise awareness about the growing threat of antibiotic-resistant gonorrhea. Let’s work together to protect our communities.