HER2 Ultra-Low Breast Cancer: Are We on the Verge of a Treatment Revolution?
Table of Contents
- HER2 Ultra-Low Breast Cancer: Are We on the Verge of a Treatment Revolution?
- The HER2 Ultra-Low Revelation
- Why This Matters to American Breast Cancer Patients
- The Diagnostic Dilemma: A call for Precision
- The Future of HER2 Testing: What to Expect
- Pros and Cons of Widespread HER2 Ultra-low Testing
- The Economic Impact: A Double-Edged Sword
- A Call to Action: Empowering Patients and Physicians
- HER2 Ultra-Low Breast Cancer: A Potential Game-Changer? Interview with Dr. Anya Sharma
Imagine a world where more breast cancer patients, previously thought to have limited treatment options, could benefit from targeted therapies. A recent study suggests this future might be closer than we think, but it also highlights some critical challenges.
The HER2 Ultra-Low Revelation
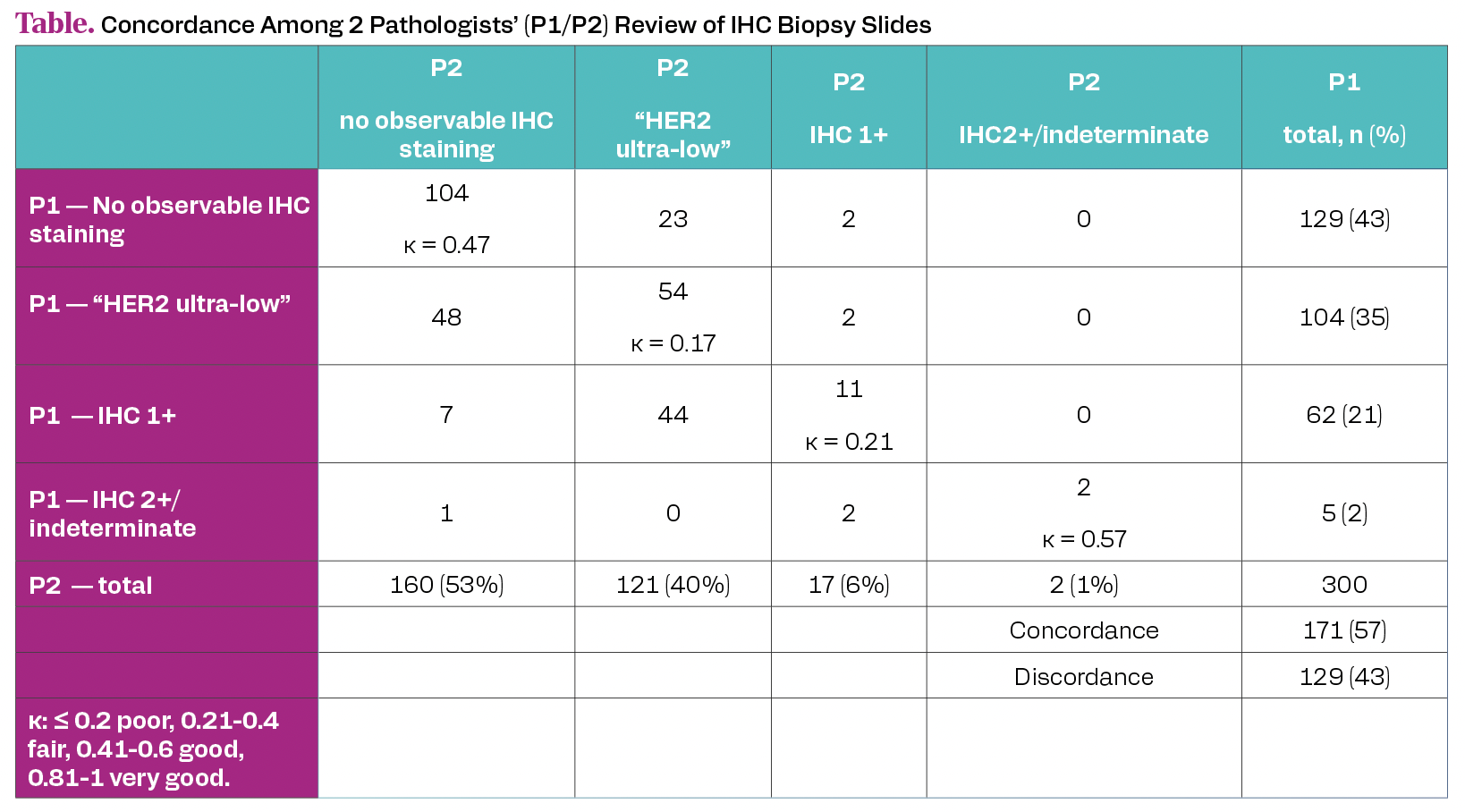
The study,conducted across three Mayo Clinic campuses,re-evaluated biopsy slides from 300 advanced breast cancer patients initially classified as HER2 IHC0. The findings? A staggering 60% were reclassified as “HER2 Ultra-Low” by at least one pathologist. This means a critically important portion of patients, once considered ineligible for HER2-targeted treatments, might actually benefit from them.
But what exactly does “HER2 Ultra-low” mean? It refers to faint membrane staining in a small percentage (between >0 and 10%) of tumor cells. This subtle expression, previously overlooked, could be the key to unlocking new treatment avenues.
Why This Matters to American Breast Cancer Patients
Breast cancer is the most common cancer among women in the united States, excluding skin cancers. According to the American Cancer Society, about 1 in 8 women will develop invasive breast cancer in their lifetime. The HER2 status of a tumor is a crucial factor in determining treatment strategies.This study suggests that current HER2 testing methods might be missing a significant subset of patients who could benefit from targeted therapies like Enhertu, which has shown promise in HER2-low breast cancer.
The Diagnostic Dilemma: A call for Precision
While the potential benefits are exciting, the study also revealed a concerning level of disagreement between pathologists in identifying HER2 Ultra-Low expression. The inter-pathologist concordance was only 57%, highlighting the subjective nature of current assessment methods. This lack of consistency could led to misdiagnosis and, consequently, inappropriate treatment decisions.
Expert Tip: If you’ve been diagnosed with HER2-negative breast cancer,discuss the possibility of HER2 Ultra-Low testing with your oncologist. A second opinion from a specialized pathologist might also be beneficial.
The Role of Artificial Intelligence and Digital Pathology
The study authors emphasize the need for increased precision in HER2 assessment. Digital pathology, coupled with artificial intelligence (AI), offers a promising solution. AI algorithms can analyze digitized biopsy slides with greater accuracy and consistency than the human eye, possibly reducing inter-observer variability and improving diagnostic reliability.
Companies like PathAI and Paige are already developing AI-powered diagnostic tools for cancer, including breast cancer. These tools could revolutionize HER2 testing, ensuring that more patients receive the right treatment at the right time.
Training and Standardization: Bridging the Gap
Beyond technology, the study underscores the importance of ongoing training for community practice pathologists. Standardizing HER2 assessment guidelines and providing pathologists with access to expert consultations can help improve diagnostic accuracy and reduce discrepancies.
Professional organizations like the American Society of Clinical Oncology (ASCO) and the Collage of American Pathologists (CAP) play a crucial role in developing and disseminating best practice recommendations for HER2 testing.
The Future of HER2 Testing: What to Expect
the findings from this study are likely to spur further research into HER2 Ultra-Low breast cancer. We can expect to see:
- Development of more sensitive and specific HER2 assays.
- Increased adoption of digital pathology and AI-powered diagnostic tools.
- Clinical trials evaluating the efficacy of HER2-targeted therapies in HER2 Ultra-Low patients.
- Updated guidelines for HER2 testing and treatment.
Pros and Cons of Widespread HER2 Ultra-low Testing
Should HER2 Ultra-Low testing become a standard practice? Let’s weigh the potential benefits and drawbacks:
Pros:
- Increased access to targeted therapies for more patients.
- Improved treatment outcomes.
- More personalized treatment plans.
Cons:
- Increased healthcare costs.
- potential for overtreatment.
- Need for specialized testing and expertise.
- Risk of false-positive results.
The Economic Impact: A Double-Edged Sword
The widespread adoption of HER2 Ultra-Low testing could have significant economic implications. While it could lead to increased spending on HER2-targeted therapies, it could also result in cost savings by preventing disease progression and reducing the need for more aggressive treatments down the line.
The Centers for Medicare & Medicaid Services (CMS) will likely play a key role in determining the reimbursement policies for HER2 Ultra-Low testing and related treatments.Their decisions will have a major impact on access to care for American breast cancer patients.
A Call to Action: Empowering Patients and Physicians
The HER2 Ultra-Low story is a reminder that our understanding of cancer is constantly evolving. By staying informed, advocating for better testing methods, and participating in clinical trials, patients and physicians can help shape the future of breast cancer treatment.
Swift Fact: Enhertu, a HER2-targeted antibody-drug conjugate, has shown remarkable efficacy in HER2-low metastatic breast cancer, offering new hope for patients with limited treatment options.
The journey to conquer breast cancer is far from over, but with continued research, innovation, and collaboration, we can create a future where every patient receives the best possible care.
Share this article to raise awareness about HER2 Ultra-Low breast cancer and its potential impact on treatment options.
HER2 Ultra-Low Breast Cancer: A Potential Game-Changer? Interview with Dr. Anya Sharma
Is HER2 Ultra-Low breast cancer a new frontier in treatment? Our editor sits down with Dr. Anya Sharma, a leading oncologist, to discuss the latest research adn what it means for patients.
Time.news Editor: Dr.Sharma, thank you for joining us. A recent study has brought HER2 Ultra-Low breast cancer to the forefront. Could you explain what HER2 Ultra-Low means, and why it’s notable?
Dr.Anya Sharma: Absolutely. For years, breast cancer has been categorized as HER2-positive, HER2-negative, or HER2-low based on the amount of HER2 protein on the surface of cancer cells. HER2 Ultra-Low is a newly defined category,referring to tumors with a very faint,subtle HER2 expression – between >0 and 10% of tumor cells showing membrane staining. This is significant as patients with these cancers were previously considered HER2-negative and ineligible for HER2-targeted therapies. The study suggests that a significant number of these patients might actually benefit from such treatments, like Enhertu, possibly expanding treatment options considerably.
Time.news Editor: The article highlights that up to 60% of advanced breast cancer patients initially classified as HER2 IHC0 were reclassified as HER2 Ultra-Low. That’s a significant number.What does this mean for American breast cancer patients currently undergoing or already having completed treatment?
Dr. Anya Sharma: This really emphasizes the need for re-evaluation. If you’ve been diagnosed with HER2-negative breast cancer, it’s worth discussing the possibility of HER2 Ultra-Low testing with yoru oncologist.Getting a second opinion on your pathology slides from a specialized pathologist familiar with HER2 Ultra-Low assessment is also advisable. It could potentially open doors to new treatment avenues. Many patients will want to know Does HER2 status affect treatment options? And the answer, with this new category is absolutely it can/does.
Time.news Editor: The study also points out a considerable diagnostic challenge: inconsistency among pathologists in identifying HER2 Ultra-low. what are the implications of this, and what can be done to improve accuracy?
Dr. Anya Sharma: This is a critical point. The subjective nature of current assessment methods can lead to misdiagnosis and incorrect treatment decisions. Improving accuracy will require a multi-pronged approach. Firstly, ongoing training and standardization of HER2 assessment guidelines for pathologists are essential. Secondly, the integration of digital pathology and artificial intelligence (AI) into the diagnostic process is promising. AI algorithms can analyze digitized biopsy slides with greater precision and consistency, reducing inter-observer variability. Companies like PathAI and Paige are at the forefront of this technology. The key is that for effective HER2 breast cancer treatment,there needs to be a uniformity in how the HER2 values are measured.
Time.news Editor: What steps do you anticipate seeing regarding HER2 breast cancer testing?
Dr. anya Sharma: First, there is the development of highly sensitive assays that can detect trace amounts of HER2 expression. In addition, with the push of testing via AI-powered platforms, test results should be more accurate and uniform. there should be additional clinical trials evaluating the efficacy of HER2-targeted therapies in the expanding HER2 Ultra-Low breast cancer group. The results of those trials, and advancements of the AI-based diagnostics will lead to updated guidelines for HER2 testing and treatment.
Time.news Editor: The article touches upon the potential “Pros and Cons” of widespread HER2 Ultra-Low testing. Can you elaborate on the potential downsides and how they can be mitigated?
Dr. Anya Sharma: While increased access to targeted therapies and improved outcomes are significant benefits, we need to be aware of potential downsides. increased healthcare costs due to more testing and treatment are a concern. Additionally, there’s a potential for overtreatment if the benefits of targeting HER2 Ultra-low are not clearly established for all patients. Therefore, it’s crucial to balance access with appropriate use, guided by clinical trials and standardized guidelines. This would also help patients with understanding their HER2 test results, and the implication on breast cancer treatment.
Time.news Editor: What’s the economic impact of this new testing?
Dr.Anya Sharma: it’s a double-edged sword economically. While the initial investment in HER2-targeted therapies will undoubtedly increase healthcare spending, the avoidance of disease progression, and the possible reduction in long-term aggressive treatments, may provide significant cost savings.The final determination of cost is up to the group that determines reimbursement policies, the Centers for Medicare & Medicaid Services (CMS).
Time.news Editor: what advice would you give to patients and physicians reading this article regarding HER2 Ultra-Low breast cancer?
Dr. Anya Sharma: For patients: be proactive. Discuss HER2 Ultra-Low testing with your oncologist if you’ve been diagnosed with HER2-negative breast cancer. Seek a second opinion if needed. Stay informed about clinical trials. For physicians: stay updated on the evolving guidelines for HER2 testing and treatment. Embrace digital pathology and AI-powered diagnostic tools as they become available. Collaborate with expert pathologists to ensure accurate assessment.
Time.news Editor: Dr. Sharma, thank you for clarifying this vital topic. Your insights are invaluable for our readers.
Dr. Anya Sharma: My pleasure. It’s crucial that patients and physicians work together to advance breast cancer treatment.