Alpha-1 Antitrypsin Deficiency (AATD): A Glimpse into the Future of Treatment
Table of Contents
- Alpha-1 Antitrypsin Deficiency (AATD): A Glimpse into the Future of Treatment
- Understanding AATD: The Silent Threat
- The Current Landscape of AATD Management
- The Dawn of Gene Therapy: A Potential Cure for AATD?
- Personalized Medicine: Tailoring Treatment to the Individual
- Early Detection: The Key to Preventing Irreversible Damage
- The Role of Technology in Transforming AATD Care
- Addressing the Challenges and Ethical Considerations
- The Future is Now: A Call to Action
- FAQ: Your Questions About AATD Answered
- Pros and Cons of Emerging AATD Treatments
- AATD Treatment: An Expert’s Take on teh Future of Alpha-1 Antitrypsin Deficiency
Imagine a world where genetic diseases like Alpha-1 Antitrypsin Deficiency (AATD) are no longer a life sentence. What if early detection and personalized treatments could dramatically alter the course of this debilitating condition? The future of AATD treatment is brimming with promise, driven by groundbreaking research and innovative therapies.
Understanding AATD: The Silent Threat
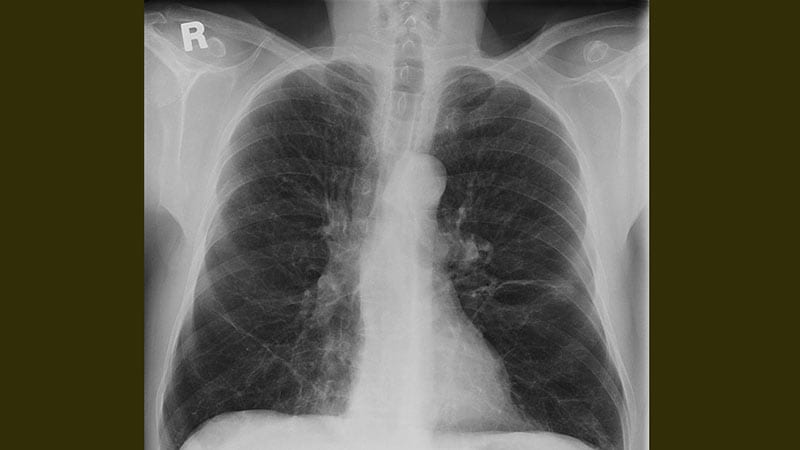
AATD, a relatively common genetic condition, often goes undiagnosed for years. This delay can have devastating consequences, as it considerably increases the risk of developing chronic obstructive pulmonary disease (COPD) and liver disease. Actually,studies suggest that 1%-5% of COPD patients may unknowingly have AATD. The insidious nature of AATD underscores the urgent need for improved diagnostic tools and more effective treatments.
The Current Landscape of AATD Management
Currently, AATD treatment primarily focuses on managing symptoms and slowing disease progression. This includes encouraging smoking cessation, treating respiratory infections, and, in some cases, administering augmentation therapy (AAT replacement). While these approaches can provide some relief, thay don’t address the underlying genetic defect.
For patients with advanced disease, more invasive interventions like volume reduction surgery or lung and liver transplantation may be considered. Though, these options come with significant risks and are not suitable for everyone.
The Dawn of Gene Therapy: A Potential Cure for AATD?
Gene therapy holds immense potential as a curative approach for AATD. the goal is to introduce a functional copy of the AAT gene into the patient’s cells, enabling them to produce the missing protein.Several gene therapy strategies are currently under investigation, including:
This approach uses modified viruses, such as adeno-associated viruses (AAVs), to deliver the AAT gene into the patient’s cells. AAVs are generally considered safe and effective for gene delivery, and they have shown promising results in preclinical studies of AATD.
CRISPR-Cas9 Gene Editing
CRISPR-Cas9 is a revolutionary gene-editing technology that allows scientists to precisely target and modify specific DNA sequences. In the context of AATD, CRISPR-Cas9 could be used to correct the mutated AAT gene directly within the patient’s cells.
mRNA Therapy
This innovative approach involves delivering messenger RNA (mRNA) encoding the AAT protein into the patient’s cells. The cells then use this mRNA template to produce the missing protein. mRNA therapy offers several advantages, including its ease of manufacturing and its transient nature, which reduces the risk of long-term side effects.
while gene therapy is still in its early stages of development, the initial results are encouraging. Clinical trials are underway to evaluate the safety and efficacy of various gene therapy approaches for AATD. If successful, gene therapy could offer a one-time, curative treatment for this debilitating condition.
Personalized Medicine: Tailoring Treatment to the Individual
The future of AATD treatment is also moving towards a more personalized approach. This involves taking into account the individual patient’s genetic makeup, disease severity, and other factors to tailor treatment strategies accordingly.
Genetic Profiling
advances in genetic testing are making it easier to identify specific AATD mutations and assess an individual’s risk of developing lung or liver disease.This information can be used to guide treatment decisions and monitor disease progression.
Biomarker Discovery
Researchers are actively searching for biomarkers that can predict disease severity and response to treatment in AATD patients. These biomarkers could help clinicians identify patients who are most likely to benefit from specific therapies and monitor their response over time.
Drug Repurposing
Drug repurposing involves identifying existing drugs that may have beneficial effects in AATD. This approach can accelerate the development of new treatments by leveraging the existing safety and efficacy data of approved drugs.
Early Detection: The Key to Preventing Irreversible Damage
Early detection is crucial for preventing the irreversible lung and liver damage associated with AATD. Unfortunately, many individuals with AATD remain undiagnosed for years, missing the chance to receive timely treatment and lifestyle counseling.
Newborn Screening
Newborn screening for AATD could identify affected individuals early in life, allowing for proactive interventions to prevent or delay the onset of disease. While newborn screening for AATD is not currently global in the United States,it is indeed being considered in some states.
Targeted Screening
Targeted screening involves testing individuals who are at high risk of having AATD, such as those with a family history of the condition or those with unexplained COPD or liver disease. This approach can help identify individuals who may have been missed by routine screening.
Increased Awareness
Raising awareness of AATD among healthcare professionals and the general public is essential for improving early detection rates. this can be achieved through educational campaigns, professional training programs, and patient advocacy efforts.
The Role of Technology in Transforming AATD Care
Technology is playing an increasingly crucial role in transforming AATD care, from diagnosis to treatment and monitoring.
Telemedicine
Telemedicine allows patients to connect with healthcare providers remotely, improving access to care for those who live in rural areas or have difficulty traveling. Telemedicine can be used for routine check-ups, medication management, and pulmonary rehabilitation.
Wearable Sensors
Wearable sensors can track various physiological parameters, such as heart rate, breathing rate, and activity levels. This data can be used to monitor disease progression, assess treatment response, and detect early signs of exacerbations.
Artificial Intelligence (AI)
AI algorithms can analyze large datasets to identify patterns and predict outcomes in AATD patients. AI can be used to improve diagnostic accuracy, personalize treatment plans, and accelerate drug discovery.
Addressing the Challenges and Ethical Considerations
While the future of AATD treatment is bright, there are several challenges and ethical considerations that need to be addressed.
Cost and Accessibility
New therapies, such as gene therapy, can be very expensive, raising concerns about cost and accessibility. It is indeed critically important to ensure that these treatments are affordable and accessible to all patients who need them.
Long-Term Safety
The long-term safety of new therapies, particularly gene therapy, needs to be carefully evaluated. Clinical trials need to follow patients for many years to monitor for any potential side effects.
Ethical Considerations of Gene Editing
Gene editing technologies, such as CRISPR-Cas9, raise ethical concerns about the potential for unintended consequences and the possibility of germline editing (making changes to DNA that can be passed down to future generations). These concerns need to be carefully considered before gene editing is widely adopted for AATD treatment.
The Future is Now: A Call to Action
The future of AATD treatment is within our reach. By investing in research, promoting early detection, and embracing innovative technologies, we can transform the lives of individuals affected by this genetic condition.It’s time to accelerate progress and bring hope to those who have been silently suffering for too long.
FAQ: Your Questions About AATD Answered
What is Alpha-1 Antitrypsin Deficiency (AATD)?
AATD is a genetic condition that can cause lung disease, liver disease, and other health problems. It is caused by a deficiency of alpha-1 antitrypsin (AAT), a protein that protects the lungs from damage.
How is AATD diagnosed?
AATD is diagnosed through a blood test that measures AAT levels. Genetic testing can also be used to identify specific AATD mutations.
What are the symptoms of AATD?
symptoms of AATD can vary depending on the severity of the condition. Common symptoms include shortness of breath, wheezing, chronic cough, and liver problems.
is there a cure for AATD?
Currently, there is no cure for AATD. However, treatments are available to manage symptoms and slow disease progression. Gene therapy holds promise as a potential cure in the future.
What is augmentation therapy?
Augmentation therapy involves administering AAT protein intravenously to increase AAT levels in the blood.This can definitely help protect the lungs from damage.
What lifestyle changes can definitely help manage AATD?
Lifestyle changes that can help manage AATD include quitting smoking, avoiding exposure to lung irritants, and maintaining a healthy weight.
Where can I find more information about AATD?
You can find more information about AATD from organizations such as the Alpha-1 foundation and the National Institutes of Health (NIH).
Pros and Cons of Emerging AATD Treatments
Gene Therapy
Pros: Potential for a one-time, curative treatment; addresses the underlying genetic defect.
Cons: High cost; potential for long-term side effects; ethical considerations related to gene editing.
Personalized Medicine
Pros: Tailored treatment strategies based on individual patient characteristics; improved treatment outcomes.
Cons: Requires advanced genetic testing and biomarker discovery; might potentially be more complex to implement.
Early Detection
Pros: Prevents irreversible lung and liver damage; allows for proactive interventions.
Cons: Requires widespread screening programs; may lead to anxiety and needless testing in some individuals.
AATD Treatment: An Expert’s Take on teh Future of Alpha-1 Antitrypsin Deficiency
time.news: Welcome, Dr.Eleanor Vance. Thank you for joining us today to discuss the evolving landscape of Alpha-1 Antitrypsin Deficiency (AATD) treatment.
Dr. Vance: It’s my pleasure to be here. AATD is a field ripe with potential, and I’m happy to shed some light on recent advancements.
Time.news: AATD often remains undiagnosed for years. Why is early detection so critical in managing Alpha-1 Antitrypsin Deficiency?
Dr. Vance: That’s an excellent starting point. The insidious nature of AATD is one of its biggest challenges. A quick fact: the median time between symptom presentation and AATD diagnosis is approximately 8 years. This delay allows irreversible lung and liver damage to occur. Early detection through newborn screening or targeted testing of high-risk individuals – those with a family history or unexplained COPD – provides the possibility for timely intervention. Lifestyle changes, such as smoking cessation and avoiding lung irritants, and augmentation therapy [1, 3] can help slow disease progression.
Time.news: What are the current treatment options available for AATD, and what are their limitations?
Dr. Vance: Currently, treatment focuses on managing the disease symptoms. This includes bronchodilators, antibiotics for respiratory infections, and quitting smoking [2]. Augmentation therapy, or AAT replacement, is also available for individuals with severe deficiency [1, 3]. However, it’s important to note that while augmentation therapy provides benefit to some patients [3], these approaches manage symptoms but don’t address the underlying genetic cause. More invasive options like lung transplants are reserved for end-stage disease and come with their own significant risks.
Time.news: Gene therapy seems to be a hot topic in AATD research. Can you elaborate on the different approaches and their potential?
Dr. Vance: Absolutely. Gene therapy holds tremendous promise as a potential cure for AATD. The goal is to introduce a functional copy of the AAT gene into the patient’s cells so that their body can correctly produce the AAT protein. There are three main strategies being explored:
Viral Vector-Based Gene Therapy: Uses modified viruses, like AAVs, to deliver the AAT gene. AAVs are considered safe and have shown promise in preclinical studies.
CRISPR-Cas9 Gene Editing: This revolutionary technology allows for precise editing of DNA. In AATD, it could be used to correct the mutated AAT gene directly within the patient’s cells.
mRNA Therapy: Delivers messenger RNA encoding the AAT protein into the patient’s cells, prompting them to produce the missing protein. This is valuable due to its ease of manufacturing and reduced risk of long-term side effects.
Although gene therapy is still in its early stages, clinical trials are actively evaluating its safety and efficacy.
Time.news: You’ve mentioned personalized medicine. How is this approach revolutionizing AATD care?
Dr. Vance: Personalized medicine is transforming AATD treatment by tailoring strategies to the individual patient.This includes genetic profiling to identify specific AATD mutations and assess the risk of lung or liver disease. Researchers are also actively searching for biomarkers that can predict disease severity and treatment response. Actually,this approach can accelerate the development of new treatments by tapping on the existing safety and efficacy data of approved drugs.
Time.news: What role does technology play in enhancing AATD management, and what are your thoughts on the utilization of Telemedicine?
Dr. Vance: Technology is playing a transformative role. Telemedicine improves access to care, especially for those in rural areas. Wearable sensors* track physiological parameters to monitor disease progression,and artificial intelligence (AI) helps analyze data to improve diagnostic accuracy and personalize treatment plans.
Time.news: What are the main challenges and ethical considerations associated with these emerging AATD therapies?
Dr. Vance: There are indeed important challenges to consider. First,cost and accessibility are paramount. New therapies, like gene therapy, can be very expensive, raising concerns about equitable access. Long-term safety is another crucial point, especially for gene therapy, requiring extensive clinical trials to monitor for potential side effects.gene editing technologies, like CRISPR-Cas9, raise ethical considerations about unintended consequences and germline editing. These concerns need careful consideration before widespread adoption, so it’s important to be careful.
Time.news: What actions can our readers take to support progress in AATD research and improve the lives of those affected?
Dr. Vance: Support AATD research and advocacy organizations like the Alpha-1 Foundation. Advocate for newborn screening and increased awareness of AATD among healthcare professionals and the public. It’s essential to accelerate progress and bring hope to those who have been silently suffering for too long, something we can definitely do together.
Time.news: Dr. Vance, thank you for sharing your expertise and insights with us today.
Dr. Vance: My pleasure. Thank you for bringing attention to this important topic.