Pancreatitis Concerns Prompt UK Health Agency Study of Weight Loss Drugs
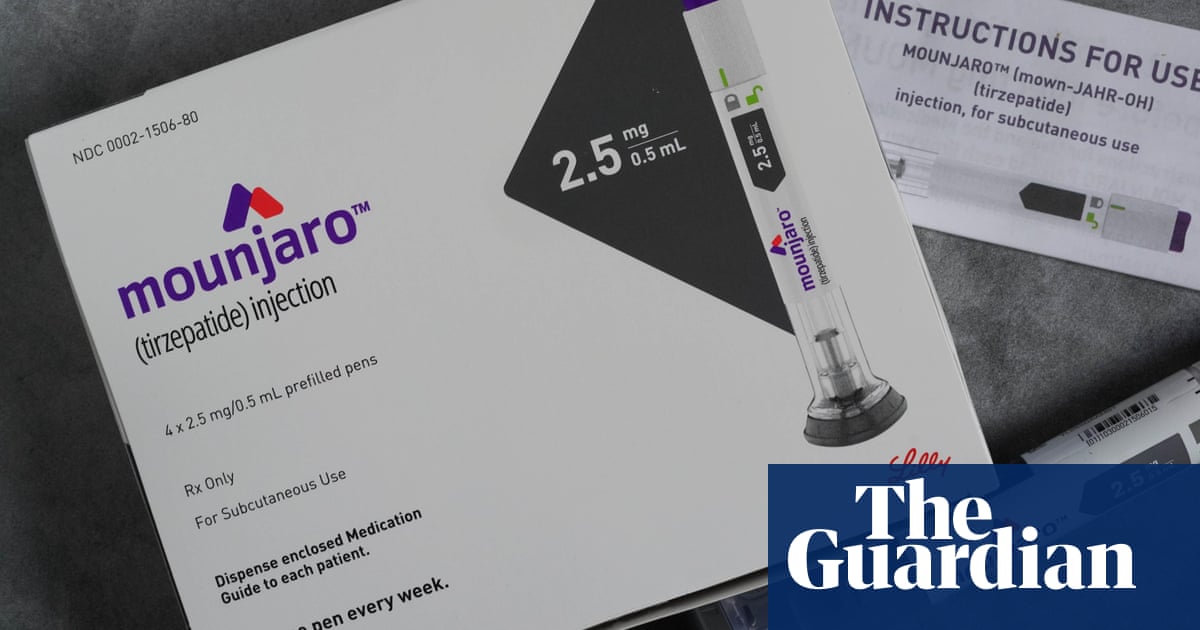
A surge in reported cases of acute pancreatitis linked to popular weight loss and diabetes medications is prompting a comprehensive investigation by UK health officials. Some cases associated with GLP-1 medicines – a class of drugs including Mounjaro, Wegovy, and Ozempic – have proven fatal, raising serious questions about the safety profile of these increasingly prescribed treatments.
The Medicines and Healthcare products Regulatory Agency (MHRA) initiated the study following a marked increase in reports submitted through its Yellow Card scheme,the UK’s system for monitoring adverse reactions to medications and medical devices. Acute pancreatitis,characterized by a sudden inflammation of the pancreas,often necessitates hospital care and presents with symptoms including severe abdominal pain,nausea,and fever.
To date, the Yellow Card scheme has received nearly 400 reports of acute pancreatitis from individuals using Mounjaro, Wegovy, Ozempic, and liraglutide. A significant portion of these reports – 181 – involve tirzepatide, the active ingredient in Mounjaro. Notably,more than one quarter of all reported cases have emerged in 2025,with 22 linked to semaglutide (Ozempic and wegovy) and 101 to tirzepatide reported since the start of the year.
“Alongside increased usage, we are seeing an upturn in the number of yellow Card reports mentioning GLP-1 medicines and acute pancreatitis,” a senior MHRA official stated.
Reader question:-If you have experienced severe side effects from a medication, what steps did you take to report it and seek medical attention?
the agency is now focusing on potential genetic factors that may predispose certain individuals to experiencing this adverse reaction. The MHRA is actively encouraging anyone hospitalized with acute pancreatitis who suspects a connection to these drugs to submit a report to the Yellow Card scheme. Healthcare professionals are also urged to report on behalf of their patients.
Patients invited to participate in the Yellow Card Biobank study, run by Genomics England, will be asked to provide detailed medical information and a saliva sample for genetic analysis.While no known genetic link currently exists, the MHRA acknowledges that individual genetic variations can influence how patients respond to medications. “Sometimes genes can influence the side-effects an individual experiences when taking a medicine,” the agency explained, “so in the context of the increasing usage of these medicines and the reports of acute pancreatitis we have received, we are exploring this further.”
Did you know?-The Yellow card scheme isn’t just for new medications. It also tracks adverse reactions to established drugs and vaccines, helping to identify previously unknown side effects.
The potential impact of adverse drug reactions on healthcare systems is substantial. Studies indicate that one in six hospital admissions are attributable to negative reactions to medication, costing the National Health Service (NHS) an estimated £2.2 billion annually in hospital stays alone.
Dr. Alison Cave, the MHRA’s chief safety officer, emphasized the potential of genetic testing in mitigating these risks.”Evidence shows that almost a third of side-effects to medicines could be prevented with the introduction of genetic testing,” she said.
Lilly,the manufacturer of Mounjaro,affirmed its commitment to patient safety. According to a company release, the company “actively monitors, evaluates and reports safety information for all our medicines.” The Mounjaro patient information leaflet already identifies acute pancreatitis as an “uncommon” side effect, affecting up to one in 100 patients, and advises individuals with a history of pancreatitis to consult their doctor before starting the medication.
This investigation underscores the importance of ongoing vigilance and comprehensive safety monitoring as the use of these powerful medications continues to expand.
unpacking teh Pancreatitis-GLP-1 Connection: A Deeper Dive
Building on the MHRA’s investigation into acute pancreatitis and GLP-1 receptor agonists (GLP-1 medicines), its crucial to understand the complexities of this potential link. As mentioned, drugs like Mounjaro, Wegovy, and Ozempic, have been the focus of increased scrutiny given the rising reports submitted to the Yellow Card scheme regarding adverse effects, including cases leading to hospitalization.
What is the relationship between GLP-1 medicines and pancreatitis? While GLP-1 receptor agonists are generally considered safe, a connection with pancreatitis has been suggested. Specifically, these drugs could perhaps increase the risk of developing pancreatitis. [[1]] Research aims to clarify whether the drugs themselves directly cause pancreatitis, or if other factors are at play.Other variables, such as the patient’s co-existing medical conditions, concomitant medications, or genetic predispositions, could play a role in the incidence of pancreatitis.
Understanding Pancreatitis: Symptoms, Causes, and Severity
Pancreatitis, as highlighted earlier, is characterized by inflammation of the pancreas. The pancreas, a vital gland, produces enzymes essential for digestion and hormones like insulin, which regulates blood sugar.Acute pancreatitis can range in severity from mild discomfort to life-threatening complications. Symptoms frequently present as severe abdominal pain that may radiate to the back, alongside nausea, vomiting, fever and, the resulting, dehydration.
- Mild Pancreatitis: Often resolves with supportive care, including pain management, intravenous fluids, and rest.
- Severe Pancreatitis: Can lead to serious complications such as organ failure, infection, and the formation of pseudocysts (fluid-filled sacs). It requires intensive care, potentially including surgery.
Numerous factors beyond GLP-1 medications can trigger pancreatitis, including:
- Gallstones: These are the most common cause.
- Alcohol Abuse: Chronic alcohol consumption considerably increases risk.
- High Triglyceride Levels: Hypertriglyceridemia can lead to pancreatitis. [[2]]
- Certain Medications: Some drugs, including those used to treat diabetes and high blood pressure, are associated with pancreatitis. [[3]]
- Genetic Predisposition: Certain genetic mutations can increase susceptibility.
Practical Tips and Monitoring
Individuals taking GLP-1 medicines should be aware of the potential risks and proactive in their health management. Here are some practical tips:
- Be Informed: Understand the potential side effects of your medication. Review the patient data leaflet and discuss any concerns with your doctor.
- Recognize symptoms: Learn to recognize the symptoms of pancreatitis and seek immediate medical attention if they occur.
- Communicate with Your Doctor: Regularly discuss your health status and any side effects with your healthcare provider.
- report Adverse Events: Report any suspected adverse reactions, including those requiring hospitalization, to the MHRA’s Yellow Card Scheme.
- monitor Other Risk Factors: Manage other risk factors for pancreatitis such as alcohol consumption, high triglyceride levels, and family history of the disease.
The ongoing MHRA investigation underscores the importance of vigilance and open interaction between patients and healthcare providers. Ongoing monitoring is key for any medication. The MHRA’s Yellow Card scheme is a crucial tool for gathering data, identifying potential risks, and ensuring patient safety.
If you experience severe abdominal pain,nausea,vomiting,and fever while taking a GLP-1 medication,seek immediate medical help. These symptoms could indicate pancreatitis or another serious condition.Early diagnosis and treatment are critical to improving outcomes and minimizing complications.
Consider reporting side effects, especially those requiring hospitalization, through the yellow card Scheme; this can help ensure prompt action and facilitate the safety monitoring of current medications.
Myths vs. Facts
It is indeed essential to address some common misconceptions regarding pancreatitis and GLP-1 medicines.
| Myth | Fact |
|---|---|
| GLP-1 medicines always cause pancreatitis. | Pancreatitis is a potential side effect, but the risk is relatively low.Many other factors can cause pancreatitis. |
| Pancreatitis from GLP-1 medicines is always severe. | The severity of pancreatitis varies. Some cases are mild and resolve with supportive care; others can be severe. |
| If you experience abdominal pain, it’s definitely pancreatitis. | Abdominal pain can have many causes. It’s vital to seek medical help but not automatically assume pancreatitis. |
Frequently Asked Questions
Here are some common questions about GLP-1 medicines and pancreatitis:
Do all GLP-1 medicines carry the same risk of pancreatitis?
Current data suggests the risk may vary slightly between different GLP-1 agonists. More research is needed to fully understand these nuances. The MHRA investigation seeks to clarify these differences.
What should I do if I suspect I have pancreatitis while taking a GLP-1 medicine?
Seek immediate medical attention. Describe all your symptoms to your doctor. Report the potential adverse reaction to the MHRA.
Can people with a history of pancreatitis take GLP-1 medicines?
Consult your doctor before starting a GLP-1 medication. Your doctor can assess your individual risk factors and determine if the medication is a safe option for you.
How long after starting a GLP-1 medicine can pancreatitis develop?
Pancreatitis can develop at any time after starting the medication. The timing can vary from patient to patient. Always be vigilant about potential side effects.
Will this investigation affect access to GLP-1 medicines?
The MHRA’s investigation aims to ensure the safe use of these medications. It is indeed unlikely to change access promptly, but findings could lead to updated prescribing guidelines or patient information.
Table of Contents