Image source, SPL
- Author, Editorial Team
- Author title, BBC News Mundo
The World Health Organization (WHO) has declared the highly infectious disease mpox as an international health emergency for the second time in two years.
Previously known as monkeypox, this condition has killed at least 450 people in a recent outbreak originating in the Democratic Republic of the Congo.
It has now spread through parts of Central and East Africa, and scientists are warning about the speed of spread and high mortality rate of the new variant.
WHO Director Tedros Adhanom Ghebreyesus stated that the possibility of further spread is “very concerning” and urged for a “coordinated international response.”
By declaring the mpox outbreak as a global health emergency, WHO aims to accelerate research, funding, and the introduction of new international public health measures.
But what is mpox? Here are some questions and answers about this contagious disease.
How common is mpox and in which countries is it found?
The mpox disease is caused by the simian smallpox virus.
This belongs to the same group of viruses as smallpox, but it is much less harmful.
The virus was originally transmitted from animals to humans, but it is now also spread between people.
Its incidence is higher in remote villages in the rainforests of Africa, in countries such as the Democratic Republic of the Congo.
These regions see thousands of cases and hundreds of deaths from the disease each year, particularly affecting children under 15 years old.
Two main strains of the virus have been detected in circulation.
“Clade 1” is endemic in Central Africa, while “clade 1b” is the new type of virus, more aggressive, responsible for the current outbreak.
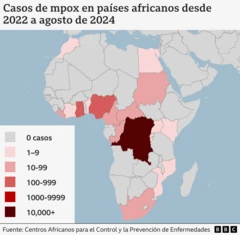
The Africa Centers for Disease Control and Prevention (CDC) reported more than 14,500 infections and over 450 deaths from mpox between early 2024 and the end of July.
This represents a 160% increase in infections and a 19% increase in deaths compared to the same period in 2023.
While 96% of mpox cases occur in the Democratic Republic of the Congo, the disease has spread to many neighboring countries such as Burundi, Kenya, Rwanda, and Uganda, where it is not considered endemic.
A milder strain of mpox known as “clade II,” which exists in West Africa, caused a global outbreak in 2022.
It spread to almost 100 countries, some of them in Europe and Asia where the virus was previously unknown, but was controlled by vaccinating vulnerable groups.
Access to mpox vaccines and treatments in the Democratic Republic of the Congo is limited, and health officials have expressed concern over the spread of the disease.
What are the symptoms?

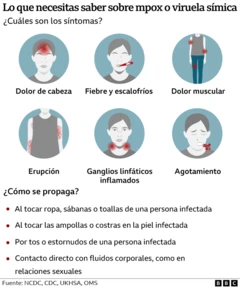
Initial symptoms include fever, headaches, swelling, back pain, and muscle aches.
When the fever subsides, rashes may appear that usually start on the face and can then spread to other parts of the body, especially the palms of the hands and the soles of the feet.
The rash, which can cause a lot of itching or pain, changes and goes through different stages before finally forming a scab that then falls off. The lesions can leave scars.
The infection usually resolves on its own and lasts between 14 and 21 days.
In severe cases, the lesions can cover the entire body, especially the mouth, eyes, and genitals.
How is it transmitted?
Mpox is transmitted between humans through close contact with someone who is infected, which includes sexual intercourse, skin-to-skin contact, and talking or breathing near another person.
The virus can enter the body through broken skin, the respiratory tract, or through the eyes, nose, or mouth.
It can also be transmitted by touching contaminated objects with the virus, such as bedding, clothing, or towels, as well as from contact with infected animals, like monkeys, rats, or squirrels.
During the global outbreak of 2022, the virus spread primarily through sexual contact.
The current outbreak in the Democratic Republic of the Congo is attributed mainly to sexual contact, but other routes have also been identified.

Who is at greater risk?
Most cases are among sexually active individuals and men who have sex with other men.
People with multiple partners or new sexual partners would be at greater risk.
However, anyone who has close contact with someone showing symptoms, such as healthcare workers and family members, can become infected with the virus.
In communities where the virus is present, it is advised to avoid close contact with anyone who has mpox and to wash hands with soap and water.
People suffering from mpox should isolate until all their lesions have healed.
WHO recommends the use of condoms as a precaution when engaging in sexual activities during the 12 weeks following recovery.
How can it be treated?
A therapy designed for smallpox may also be useful for mpox, but research on its effectiveness is limited.
Mpox outbreaks can be controlled through prevention, and the best way to do this is with vaccines.
There are three vaccines, but they are generally only available for at-risk individuals or those who have had close contact with an infected person.
Currently, WHO does not recommend vaccination of entire populations.
More vaccine trials against new strains of mpox are needed to accurately assess how much protection they provide.
Recently, WHO called on pharmaceutical companies to submit their mpox vaccines for emergency use, even if those vaccines have not been formally approved in the countries where they are needed.
And remember, you can receive notifications in our app. Download the latest version and enable them.
