“`html
The Future of emergency Medicine: From Overwhelmed to Optimized
Table of Contents
- The Future of emergency Medicine: From Overwhelmed to Optimized
- The Crisis in Emergency Rooms: A growing Problem
- The Rise of the Urgenciologist: A Model for the Future?
- Technology to the Rescue: Innovations Transforming Emergency Care
- Addressing Territorial Inequality: Bringing Quality Care to All
- The Ethical Dimensions of Emergency Medicine: Decisions in the First Minute
- The Future of Emergency Medicine Training: Preparing the Next Generation
- FAQ: Your questions About the Future of emergency Medicine Answered
- The Future of Emergency Medicine: An Expert’s Perspective
Imagine walking into an emergency room and being seen immediately by a specialist, armed wiht the latest technology and a perfectly coordinated team.Is this a pipe dream? Not necessarily.The challenges facing emergency medicine today, from overcrowding to staffing shortages, are driving innovation and sparking a revolution in how we deliver critical care. Let’s dive into what the future might hold,drawing lessons and inspiration from global trends and applying them to the American landscape.
The Crisis in Emergency Rooms: A growing Problem
Emergency rooms across the United States are facing a perfect storm.Increased patient volume, aging populations, and a shortage of qualified emergency medicine physicians are pushing the system to its breaking point.Just like in Chile, where emergency consultations surged by 45% between 2020 and 2024 [[article], American ERs are seeing a similar, if not more pronounced, increase. This surge is fueled by factors like:
- Post-Pandemic Effects: The lingering health issues and delayed care from the COVID-19 pandemic continue to strain resources.
- Aging Population: As baby boomers age, the demand for emergency services increases due to chronic conditions and age-related illnesses.
- Primary Care Shortages: Lack of access to primary care forces many to seek treatment in the ER for non-emergency conditions.
The consequences are dire: longer wait times, increased patient mortality, and burnout among healthcare professionals. The Chilean Medical Magazine‘s 2025 analysis highlights saturation, bed deficits, and territorial inequality [[article] – issues that resonate deeply within the American healthcare system as well.
The Rise of the Urgenciologist: A Model for the Future?
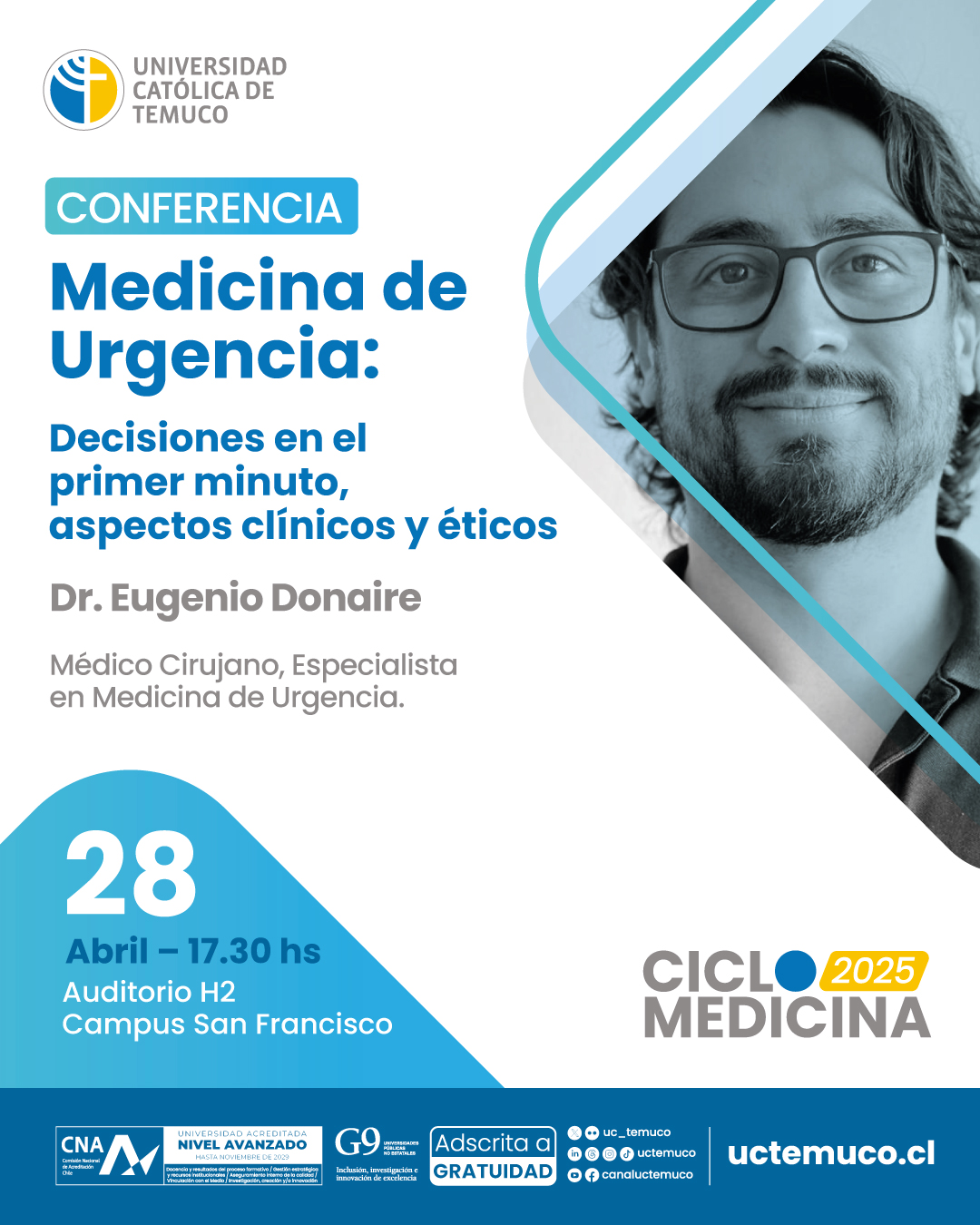
Dr. Eugenio Donaire Vera, a leading emergency medicine specialist in Chile, emphasizes the importance of specialized leadership in emergency care [[article]. He argues that while general practitioners are valuable, an “urgenciologist” – a physician specifically trained in emergency medicine – is crucial for guiding the team and making critical decisions under pressure. This concept is gaining traction in the US, with a growing emphasis on board-certified emergency medicine physicians leading ER teams.
The American Board of Emergency Medicine (ABEM): Setting the Standard
The ABEM certifies physicians who have met rigorous training and knowledge requirements in emergency medicine. Having ABEM-certified physicians in leadership roles ensures a higher standard of care and improved patient outcomes. Hospitals are increasingly prioritizing ABEM certification when hiring emergency medicine staff.
The Importance of Teamwork and Communication
Dr.Donaire highlights the critical role of teamwork and communication in emergency situations [[article]. He stresses that a good leader must effectively organize and communicate with all members of the healthcare team,from nurses to students.This emphasis on teamwork is echoed in American emergency medicine, where interdisciplinary collaboration is seen as essential for efficient and effective care.
Technology to the Rescue: Innovations Transforming Emergency Care
Technology is poised to revolutionize emergency medicine, offering solutions to many of the challenges facing ERs today. From artificial intelligence to telemedicine, these innovations have the potential to streamline processes, improve patient outcomes, and alleviate the burden on healthcare professionals.
Artificial Intelligence (AI): The Smart ER
AI is being used in a variety of ways to improve emergency care:
- Triage and Diagnosis: AI algorithms can analyze patient data, such as vital signs and symptoms, to quickly assess the severity of their condition and prioritize treatment. This can significantly reduce wait times and ensure that the sickest patients are seen first.
- Predictive Analytics: AI can predict potential surges in patient volume, allowing hospitals to proactively allocate resources and staff.
- Decision Support: AI-powered tools can provide physicians with real-time access to the latest medical research and guidelines, helping them make more informed decisions.
Such as, companies like Google and IBM are developing AI-powered diagnostic tools that can assist physicians in identifying conditions such as stroke and sepsis in the early stages, when treatment is most effective.
Telemedicine: Expanding Access to Care
Telemedicine is breaking down geographical barriers and expanding access to emergency care, particularly in rural areas where access to specialists is limited. Through video conferencing and remote monitoring, physicians can assess patients, provide consultations, and even guide emergency medical technicians (EMTs) in the field.
The University of Pittsburgh Medical Centre (UPMC) is a leader in telemedicine, offering a wide range of virtual emergency care services, including telestroke and tele-ICU programs. These programs have been shown to improve patient outcomes and reduce hospital readmission rates.
Wearable Technology: Monitoring Patients Remotely
Wearable devices, such as smartwatches and fitness trackers, are becoming increasingly elegant, capable of monitoring vital signs, detecting falls, and even alerting emergency services in the event of a medical emergency. This technology can be particularly valuable for elderly patients and those with chronic conditions.
Apple Watch, for example, has a fall detection feature that can automatically call 911 if the user is unresponsive after a fall. This feature has already saved countless lives.
Addressing Territorial Inequality: Bringing Quality Care to All
As the Chilean Medical Magazine points out, territorial inequality is a important challenge in emergency medicine [[article]. Patients in rural areas often face longer wait times, limited access to specialists, and inadequate resources. Addressing this inequality requires a multi-pronged approach:
Investing in Rural Healthcare Infrastructure
Federal and state governments need to invest in upgrading healthcare infrastructure in rural areas, including hospitals, clinics, and emergency medical services. This includes providing funding for new equipment,technology,and staffing.
Incentivizing Physicians to Practice in Rural Areas
Many physicians are reluctant to practice in rural areas due to lower salaries, limited career opportunities, and social isolation. To address this, governments can offer financial incentives, such as student loan forgiveness programs and tax breaks, to encourage physicians to practice in underserved communities.
Expanding Telemedicine Services
Telemedicine can play a crucial role in bridging the gap in access to care between urban and rural areas. By expanding telemedicine services, patients in rural areas can receive timely consultations and treatment from specialists, without having to travel long distances.
The Ethical Dimensions of Emergency Medicine: Decisions in the First Minute
Dr. Donaire emphasizes the ethical considerations that arise in emergency medicine, particularly the need to make critical decisions in the first minute of care [[article]. These decisions can have life-or-death consequences, and physicians must be prepared to act quickly and decisively, while also respecting patient autonomy and ethical principles.
Whenever possible, physicians should obtain informed consent from patients before initiating treatment. However, in emergency situations, when patients are unable to provide consent, physicians must act in the patient’s best interests, based on their professional judgment and ethical guidelines.
Resource Allocation and Triage
In situations where resources are limited,physicians must make difficult decisions about how to allocate those resources. Triage protocols are used to prioritize patients based on the severity of their condition, ensuring that the sickest patients receive the most immediate attention.
End-of-Life Care
Emergency physicians frequently enough encounter patients who are near the end of their lives.In these situations, it is significant to provide compassionate and respectful care, while also honoring the patient’s wishes regarding end-of-life treatment.
The Future of Emergency Medicine Training: Preparing the Next Generation
The future of emergency medicine depends on the quality of training that is provided to the next generation of physicians. Emergency medicine training programs must adapt to the changing landscape of healthcare, incorporating new technologies, addressing ethical challenges, and emphasizing teamwork and communication skills.
Simulation-Based Training
Simulation-based training is becoming increasingly popular in emergency medicine, allowing physicians to practice critical skills in a safe and controlled surroundings. Simulation scenarios can be used to replicate a wide range of emergency situations, from cardiac arrest to trauma.
Interprofessional Education
Interprofessional education brings together students from different healthcare disciplines, such as medicine, nursing, and pharmacy, to learn and work together. This type of training helps to foster teamwork and communication skills, which are essential for effective emergency care.
Global Health Experiences
Global health experiences can provide emergency medicine residents with valuable opportunities to learn about different healthcare systems and cultures. These experiences can broaden their perspectives and help them to become more culturally competent physicians.
FAQ: Your questions About the Future of emergency Medicine Answered
What are the biggest challenges facing emergency medicine today?
The biggest challenges include overcrowding, staffing shortages, territorial inequality (unequal access to care), and the increasing complexity of patient needs due to an aging population and the lingering effects of the pandemic.
How can technology improve emergency care?
Technology like AI can improve triage,diagnosis,and resource allocation.Telemedicine expands access to care in rural areas, and wearable devices allow for remote patient monitoring.
what is the role of leadership in emergency medicine?
Strong leadership, ideally from board-certified emergency medicine physicians, is crucial for organizing the healthcare team, making critical decisions under pressure, and ensuring a high standard of care.
The Future of Emergency Medicine: An Expert’s Perspective
Emergency rooms are vital components of our healthcare system,but they face numerous challenges. We sat down with Dr. Anya Sharma, a leading expert in emergency medicine, to discuss the innovations and strategies shaping the future of critical care. Here’s what she had to say.
Q&A with Dr. Anya Sharma
Time.news Editor: Dr. Sharma, thank you for joining us. Emergency rooms across the US seem to be under immense pressure. What are the most notable challenges they face today?
Dr. Anya Sharma: It’s a pleasure to be here.You’re right, our emergency rooms are indeed facing a perfect storm. We’re seeing increased patient volumes, an aging population with more complex health needs, and persistent staffing shortages. The post-pandemic effects are still straining our resources,and a lack of access to primary care often pushes people to seek emergency care for non-emergency conditions.
Time.news Editor: The article mentions a surge in emergency consultations similar to what happened in Chile. How do these global trends inform what’s happening here in the US?
Dr. Anya Sharma: absolutely. The Chilean experience,with a 45% surge in emergency consultations,highlights a universal problem: healthcare systems worldwide are struggling to meet demand. the “Chilean Medical Magazine” analysis pointing to saturation, bed deficits, and territorial inequality really resonates with the issues we’re seeing in the American healthcare system. It underscores the need for innovative solutions that are applicable globally.
Time.news Editor: The concept of the “urgenciologist” is intriguing. Can you elaborate on the role of specialized leadership in emergency care?
Dr. Anya Sharma: the idea, championed by Dr. Eugenio Donaire Vera, emphasizes that while general practitioners are valuable, having physicians specifically trained in emergency medicine – “urgenciologists” – leading the team is crucial. These specialists are equipped to make critical decisions under pressure and guide the healthcare team effectively. In the US, this translates to prioritizing board-certified emergency medicine physicians from the American Board of emergency Medicine (ABEM) in leadership roles. Their rigorous training ensures a higher standard of care and improved patient outcomes.
Time.news Editor: Teamwork and interaction are highlighted as essential. What practical steps can hospitals take to improve these aspects?
Dr. Anya sharma: Teamwork and communication can’t be overstated.A good leader must be able to effectively organize and communicate with everyone, from nurses to students. We recommend implementing regular team training exercises, such as simulations of critical emergency scenarios, to improve coordination and communication. These simulations create a safe environment for practice and help uncover areas for enhancement.
Time.news Editor: Let’s talk about technology. How is artificial intelligence (AI) transforming emergency care?
Dr. Anya Sharma: Technology holds immense promise for revolutionizing emergency medicine. AI is being used in several ways: for triage and diagnosis, where algorithms analyse patient data to quickly assess severity; for predictive analytics to forecast surges in patient volume; and for decision support, providing physicians with real-time access to the latest research and guidelines.Companies like Google and IBM are developing AI-powered diagnostic tools that can definitely help identify conditions like stroke and sepsis early on, when treatment is most effective. [1]
Time.news Editor: Telemedicine is also mentioned.What role does it play in expanding access to emergency care?
Dr.Anya Sharma: Telemedicine is breaking down geographical barriers and expanding access, particularly in rural areas where access to specialists is limited. Through video conferencing and remote monitoring, physicians can assess patients, provide consultations, and even guide EMTs in the field. UPMC is a great example, offering virtual emergency care services like telestroke and tele-ICU programs that have improved patient outcomes and reduced readmission rates.
Time.news Editor: Territorial inequality is a significant concern. How can we ensure that quality care is accessible to all, regardless of location?
dr. Anya Sharma: Addressing territorial inequality requires a multi-pronged approach. we need to invest in upgrading healthcare infrastructure in rural areas, including hospitals, clinics, and emergency medical services. Governments can offer financial incentives, such as student loan forgiveness programs and tax breaks, to encourage physicians to practice in underserved communities. Expanding telemedicine services is also crucial, as it allows patients in rural areas to receive timely consultations and treatment from specialists without traveling long distances. The Health Resources and services Governance (HRSA) also offers a variety of programs to support rural healthcare.
Time.news Editor: Emergency physicians frequently enough face ethical dilemmas. What are some of the key ethical considerations in emergency medicine?
Dr. anya Sharma: Emergency physicians must be prepared to make life-or-death decisions quickly, while also respecting patient autonomy and ethical principles. Informed consent is crucial whenever possible, but in emergency situations where patients can’t provide consent, physicians must act in their best interests. Resource allocation and triage are also critical ethical considerations, especially when resources are limited.Additionally, emergency physicians