Extubation Failure: An Overlooked Crisis and the Path to Prevention
Table of Contents
- Extubation Failure: An Overlooked Crisis and the Path to Prevention
- Extubation Failure: Interview with Dr. Anya Sharma on Prevention and the Future of Airway Management
Imagine a patient finally breathing on their own, only to face respiratory distress again within hours. Extubation failure, the inability to maintain spontaneous breathing after removal of a breathing tube, is a silent crisis in American hospitals, impacting patient outcomes and driving up healthcare costs. But what if we could predict and prevent it?
Understanding the Scope of the Problem
Extubation failure isn’t a rare event. Studies show it occurs in a important percentage of patients,leading to reintubation,prolonged ICU stays,and increased mortality. This isn’t just a statistic; it represents real peopel facing potentially avoidable complications.
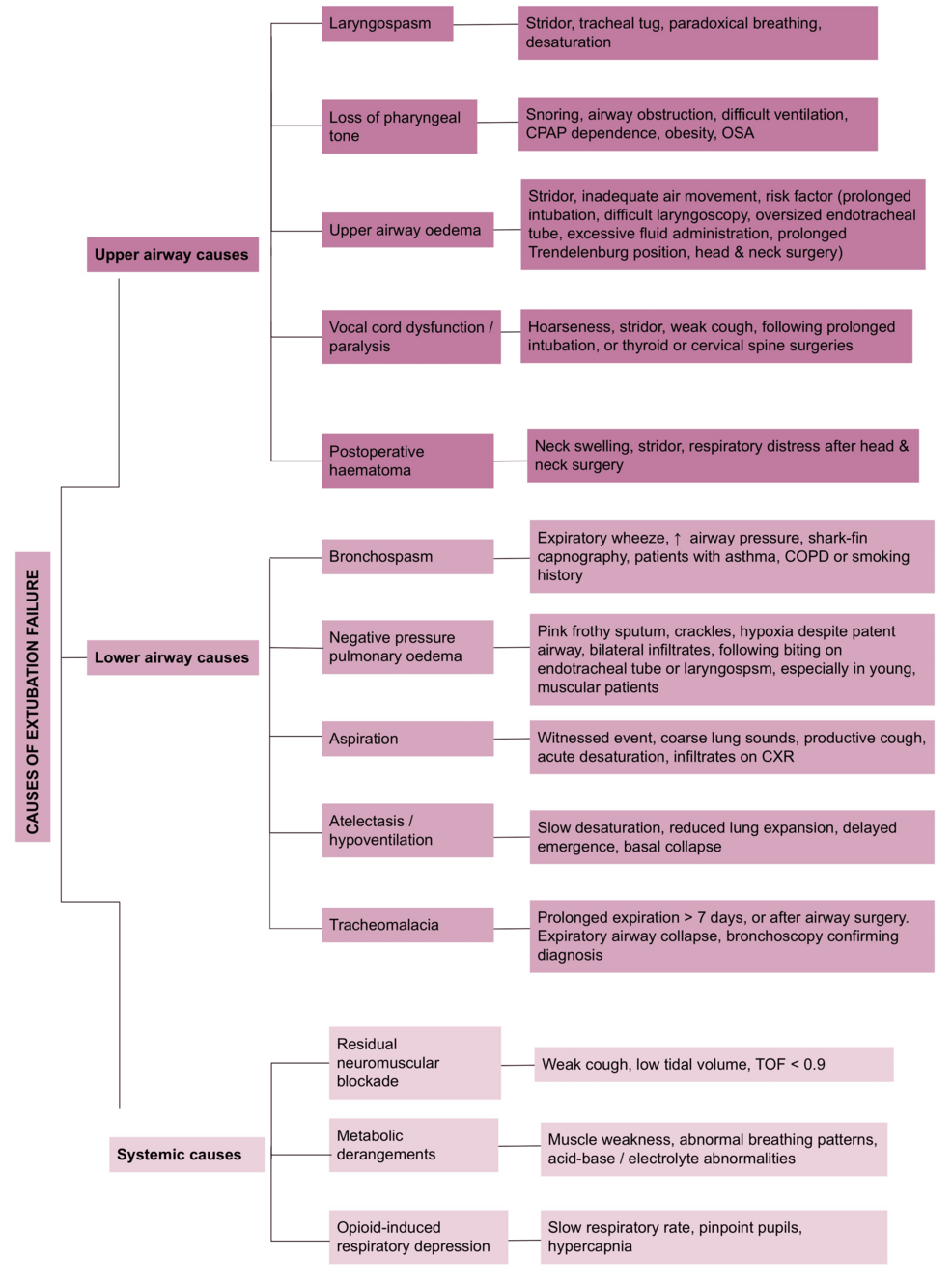
Why Does Extubation Fail?
Several factors contribute to extubation failure. These include:
- Weak Respiratory Muscles: Patients who have been on ventilators for extended periods can experiance muscle weakness, making it difficult to breathe independently.
- Airway Obstruction: Swelling or othre obstructions in the airway can impede airflow.
- Underlying Medical Conditions: Conditions like pneumonia,heart failure,or chronic obstructive pulmonary disease (COPD) can compromise respiratory function.
- Inadequate Assessment: Failing to properly assess a patient’s readiness for extubation can lead to premature removal of the breathing tube.
The Economic Burden of Extubation Failure
Beyond the human cost,extubation failure places a significant strain on the healthcare system. Reintubation requires additional resources, including staff time, equipment, and ICU beds, driving up costs for hospitals and patients alike. In a healthcare landscape increasingly focused on value-based care, preventing extubation failure is not just good medicine; it’s good economics.
Future Directions in Airway Management
The good news is that researchers and clinicians are actively working to improve extubation success rates. Here are some promising areas of growth:
Advanced Monitoring Technologies
New monitoring technologies are emerging that can provide real-time insights into a patient’s respiratory function. These tools can help clinicians identify subtle signs of impending respiratory distress before they escalate into full-blown extubation failure.
Personalized extubation Protocols
one-size-fits-all approaches to extubation are becoming a thing of the past. Future protocols will likely be tailored to individual patient characteristics, taking into account factors like age, underlying medical conditions, and duration of mechanical ventilation.This personalized approach can definitely help ensure that patients are only extubated when they are truly ready.
the Role of Artificial Intelligence (AI)
AI has the potential to revolutionize airway management. Machine learning algorithms can analyze vast amounts of patient data to predict the likelihood of extubation failure. This information can then be used to guide clinical decision-making and optimize extubation strategies.
For example, imagine an AI system that continuously monitors a patient’s vital signs, respiratory parameters, and medical history. If the system detects patterns that suggest an increased risk of extubation failure, it can alert clinicians, allowing them to intervene proactively.
Non-Invasive Ventilation (NIV) Strategies
NIV can play a crucial role in preventing reintubation after extubation. By providing respiratory support without the need for a breathing tube, NIV can help patients maintain adequate oxygenation and ventilation while their respiratory muscles recover. Though,it’s crucial to select the right patients for NIV and to monitor them closely for signs of failure.
The Importance of Multidisciplinary Collaboration
Preventing extubation failure requires a collaborative effort involving physicians, nurses, respiratory therapists, and other healthcare professionals. By working together,these teams can develop and implement comprehensive strategies to optimize patient outcomes.
What are the main risk factors for extubation failure?
The main risk factors include weak respiratory muscles, airway obstruction, underlying medical conditions like COPD or heart failure, and inadequate assessment of patient readiness.
How can AI help prevent extubation failure?
AI can analyze patient data to predict the likelihood of extubation failure, allowing clinicians to intervene proactively and optimize extubation strategies.
Real-world Examples: Success Stories and lessons Learned
Several hospitals across the United States have implemented triumphant strategies to reduce extubation failure rates. Such as, some institutions have adopted standardized extubation protocols that include rigorous assessment of respiratory muscle strength and airway patency. others have implemented early mobilization programs to help patients regain muscle strength and improve respiratory function.
One notable example is the University of Michigan Health System, which implemented a comprehensive extubation bundle that included daily assessment of readiness to wean, spontaneous breathing trials, and early mobilization. This initiative resulted in a significant reduction in extubation failure rates and improved patient outcomes.
The Future is in Prevention
Extubation failure is a complex problem with potentially devastating consequences. Though, by embracing new technologies, adopting personalized approaches, and fostering multidisciplinary collaboration, we can substantially improve extubation success rates and ensure that more patients can breathe freely and safely after coming off mechanical ventilation. The future of airway management lies in proactive prevention, not reactive intervention.
Extubation Failure: Interview with Dr. Anya Sharma on Prevention and the Future of Airway Management
Time.news: Dr. Sharma, thank you for joining us. Extubation failure, the inability too breathe independently after removing a breathing tube, is gaining attention. Why is this such a critical issue in hospitals today?
dr. Anya Sharma: it’s a pleasure to be here. Extubation failure is indeed a meaningful concern. It’s not just a technical hiccup; it significantly impacts patient outcomes. We’re talking about increased risk of reintubation [2], prolonged ICU stays, higher mortality rates, and increased healthcare costs. It’s a cascade of negative consequences we can,and should,be working to prevent. It’s important to note that international guidelines advocate for non-invasive ventilation after extubation for high-risk patients as it can reduce respiratory failure, the need for reintubation, and even mortality [1].
Time.news: The human and financial costs are clearly substantial. What are the primary factors that lead to extubation failure?
Dr.Anya Sharma: Several factors can contribute. Weak respiratory muscles are a big one, especially in patients who’ve been on ventilators for an extended period. airway obstruction, whether from swelling or other causes, is another. Underlying medical conditions like pneumonia, heart failure, or COPD also play a role. Crucially, inadequate assessment of a patient’s readiness for extubation is a significant contributor. We need to be sure patients are truly ready before removing the breathing tube.
Time.news: What are the new monitoring technologies that can provide real-time insights into a patient’s respiratory function?
Dr. Anya Sharma: We’re seeing exciting advancements in monitoring technologies. devices that measure diaphragm function and respiratory muscle strength are particularly valuable. These provide detailed facts about a patient’s ability to breathe independently and can help identify subtle signs of impending respiratory distress early on.
Time.news: The article mentions personalized extubation protocols. How woudl these differ from current practices?
Dr. Anya Sharma: The customary one-size-fits-all approach is becoming outdated.Personalized protocols tailor the extubation strategy to the individual patient. This means considering factors like age, underlying medical conditions, duration of mechanical ventilation, and overall physiological status. This personalized approach ensures extubation occurs only when the patient is truly prepared.
Time.news: Artificial intelligence (AI) is also mentioned as a potential game-changer. Can you elaborate on how AI could help prevent extubation failure?
Dr. Anya Sharma: AI has the potential to revolutionize how we approach airway management. Machine learning algorithms can analyze vast amounts of patient data – vital signs, respiratory parameters, medical history – to predict the likelihood of extubation failure. This information can then guide clinical decision-making and optimize extubation strategies. Imagine an AI system continuously monitoring a patient and alerting clinicians to subtle patterns indicating increased risk, allowing for proactive intervention.
Time.news: Non-invasive ventilation (NIV) is highlighted as a key strategy. What role does NIV play in preventing reintubation after extubation?
Dr. Anya Sharma: NIV provides respiratory support without needing a breathing tube. It helps patients maintain adequate oxygenation and ventilation while their respiratory muscles recover after extubation.It’s a crucial tool, but patient selection is key. Close monitoring is essential to identify any signs of NIV failure and the potential need for reintubation.
Time.news: The article stresses the importance of multidisciplinary collaboration. Why is this so critical in preventing extubation failure?
Dr. Anya Sharma: Preventing extubation failure demands a coordinated effort. Physicians, nurses, respiratory therapists, and other healthcare professionals must work collaboratively. This team approach allows for the progress and implementation of thorough strategies, ensuring all aspects of patient care are optimized for triumphant extubation. The review of the available evidence also aims at the same goal of minimizing extubation failure [3].
Time.news: Are there any successful examples of hospitals implementing strategies to reduce extubation failure rates?
Dr. Anya Sharma: Absolutely. The University of Michigan Health System, for instance, implemented a comprehensive extubation bundle including daily readiness assessment, spontaneous breathing trials, and early mobilization. This resulted in a significant reduction in extubation failure rates and improved patient outcomes. Standardized extubation protocols with rigorous assessment of respiratory muscle strength and airway patency,alongside early mobilization programs,are proving valuable in many institutions.
Time.news: What is your final message for hospitals and clinicians looking to improve their extubation success rates?
Dr. Anya Sharma: Embrace new technologies, adopt personalized approaches, and foster multidisciplinary collaboration. Extubation failure is a complex problem, but with proactive prevention strategies in place, we can significantly improve patient outcomes and ensure more individuals can breathe freely and safely after mechanical ventilation. The future of airway management lies in prevention, not reaction.