Parasitic Worms Found in Two Kidney Transplant Recipients Linked to Single Donor
A rare and alarming case involving two kidney transplant recipients has highlighted the potential for parasitic infections to be transmitted through organ donation. The incident, detailed in a report published in the New England Journal of Medicine on June 18, 2025, underscores the critical need for enhanced screening protocols and inter-hospital communication.
Two men, aged 61 and 66, both received kidneys from the same donor who previously resided in the Caribbean. Both subsequently developed severe complications indicative of a parasitic infection, prompting a complex medical investigation.
Initial Symptoms and Diagnostic Challenges
The first patient, a 61-year-old man treated at Massachusetts General Hospital (MassGen), began experiencing a constellation of symptoms approximately 10 weeks after his transplant. These included nausea, vomiting, excessive thirst, stomach discomfort, back pain, and fever. Doctors initially discovered fluid accumulation in his lungs, leading to shortness of breath and declining oxygen levels.
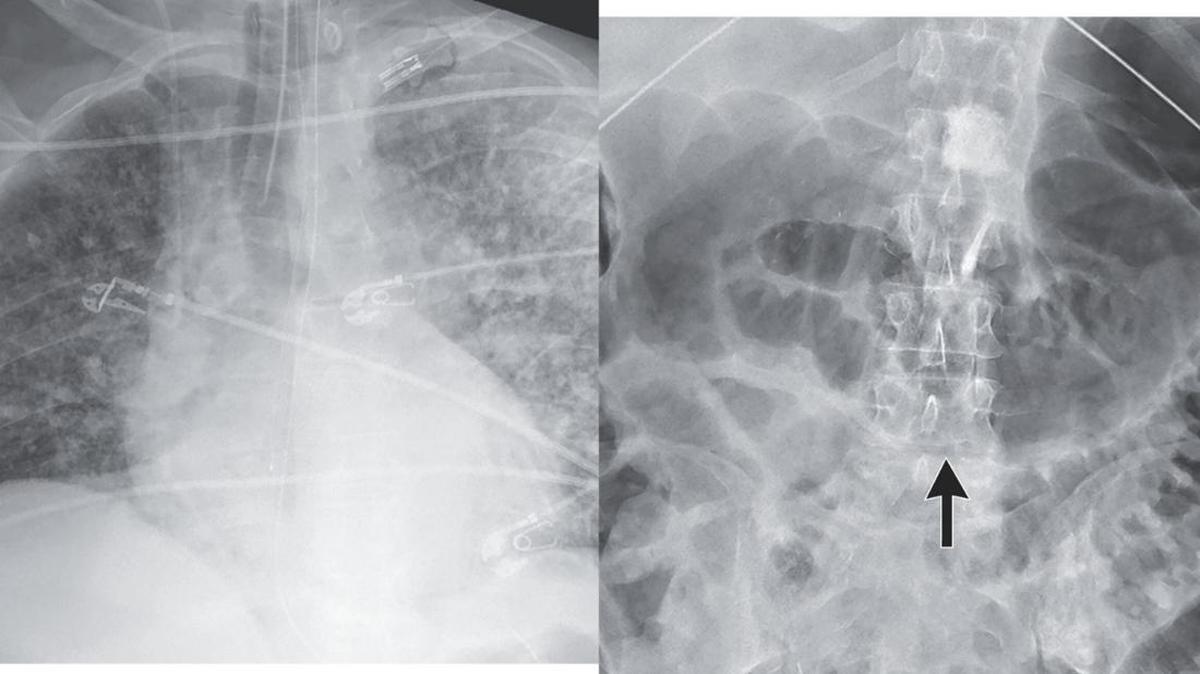
The patient’s condition rapidly deteriorated, requiring admission to the intensive care unit due to breathing failure and shock – a state characterized by dangerously low blood pressure. Medical staff observed purple, bruise-like rashes developing on his abdomen. A comprehensive investigation was launched, complicated by the patient’s use of immunosuppressive drugs, which, while necessary to prevent organ rejection, also increase vulnerability to infection.
“The medical team faced a significant challenge in differentiating between a wide range of potential infections,” explained Dr. Camille Kotton, an organ transplant specialist and infectious disease expert involved in the case. Initial tests ruled out bacterial and viral causes, including COVID-19. However, a rising level of eosinophils – a type of white blood cell that typically indicates a parasitic infection – provided a crucial clue.
Identifying the Parasite: Strongyloides Stercoralis
Suspecting a parasitic infection, doctors contacted the New England Donor Services, a regional organ procurement organization. They inquired about the possibility of contamination with Strongyloides Stercoralis, a small intestinal worm. Even after a donor’s death, blood samples can be tested for antibodies indicating prior exposure to the parasite.
Testing revealed the recipient had no antibodies to Strongyloides before the transplant, but developed them afterward. Further analysis confirmed the presence of the worm had spread throughout the patient’s body, affecting his stomach, lungs, and skin.
The MassGen team successfully treated the patient with ivermectin, a potent antiparasitic medication. Special permission was obtained to administer the drug directly under the skin, maximizing its effectiveness in combating the systemic infection.
A Second Case Emerges and Collaborative Response
Meanwhile, Albany Medical Center was treating a 66-year-old man who had also received a kidney from the same donor. This patient presented with lower white blood cell counts and declining kidney function post-transplant. Recognizing the similarities to the MassGen case, doctors shared their findings, leading to a swift diagnosis and treatment plan.
“Organ transplants save lives,” stated a spokesperson for Albany Medical Center. “In a rare case like this, communication and coordination between our hospitals, along with the involvement of infectious disease specialists and alerts from our regional organ procurement organization, were vitally important.”
This incident serves as a stark reminder of the complexities of organ transplantation and the importance of vigilance in safeguarding the health of recipients. The collaborative response between MassGen and Albany Medical Center ultimately ensured positive outcomes for both patients, but it also highlights the need for ongoing refinement of donor screening procedures to prevent similar occurrences in the future.
The Expanding Scope of Transplant-Associated Infections
the alarming cases of parasitic infections in kidney transplant recipients, as reported in the New England Journal of Medicine, highlight a critical area of focus in transplant medicine. While the swift diagnosis and treatment were crucial in thes instances, the incident underscores the need for ongoing improvements in donor screening and recipient care. This includes a deeper look at the parasites capable of transmission, not just Strongyloides stercoralis.
Beyond Strongyloides: Othre Parasites of Concern
The medical community is now more aware that organ transplants can transmit various parasitic infections. Several other parasites, like Trypanosoma cruzi (Chagas disease), Toxoplasma gondii (Toxoplasmosis), and various species of malaria, pose significant risks. These infections,if undiagnosed and untreated,can lead to severe complications in transplant recipients due to their weakened immune systems.
The source of infection from the donor is often related to the geographic location of the donor. Individuals from areas where specific parasitic diseases are endemic are those at the highest risk. Organ procurement organizations (OPOs) are now increasing their scrutiny of donor location history to mitigate these risks.
Enhanced screening protocols are essential. This involves complete blood tests, assessing for antibodies or, ideally, the direct detection of parasites. The tests should be based on the donor’s travel history and likely exposures. More advanced molecular testing methods can detect parasitic DNA or RNA,even when antibody tests are inconclusive.
Challenges in Diagnosis and treatment of Parasitic Infections
Diagnosing parasitic infections in transplant recipients is challenging due to the use of immunosuppressive drugs. These medications can mask symptoms and make it difficult to differentiate parasitic infections from other post-transplant complications, such as infections and rejection.
Treatment can be complex. The antiparasitic medications, like ivermectin used in the cases above, can have side effects and potential interactions with immunosuppressants. Moreover, some parasites are resistant to common treatments, leading to the need for specialized therapies.
The use of immunosuppressive medications directly impacts the body’s ability to fight infections. The goal is to strike a balance,preventing organ rejection while minimizing the risk of severe infections.This requires constant monitoring, dose adjustments, and, in some cases, prophylactic medications to prevent infection.
Practical Steps to Mitigate Risk
To prevent these devastating outcomes, transplant centers and patients must take certain steps. These include:
- Detailed Donor History: Thorough inquiries into the donor’s travel history, especially to areas with a high prevalence of parasitic diseases.
- Comprehensive Screening: Implementing a broader range of tests to detect potential parasitic infections in donors.
- Rapid Diagnosis: Utilizing advanced diagnostic methods, including molecular testing, to detect infections early.
- Prophylactic Treatment: In certain cases, administering medications to prevent known, high-risk infections in recipients from transplanting from donors known to have parasites.
- Patient Education: Making sure transplant recipients understand the risks and symptoms of parasitic infections. This should include information on who to contact and what to do if symptoms arise after transplant.
- Inter-Hospital Collaboration: Like the MassGen and Albany Medical Center example,hospitals must establish clear dialog channels to share information about unusual cases and potential donor-related infections.
The Future of Transplant Safety
The cases of Strongyloides stercoralis infection demonstrate the need for increased vigilance in organ donation. A proactive approach integrating improved screening, diagnostic tools, and enhanced communication will minimize the risk of parasitic infections in transplant recipients. By staying informed and adapting to new challenges,the medical community can improve patient outcomes and the safety of organ transplantation.
Collaboration between transplant centers, OPOs, and infectious disease specialists remains paramount to safeguarding patients. This team approach, coupled with ongoing research, will pave the way for a safer future for transplant recipients, allowing them to receive the life-saving benefits of organ donation with minimized risk.
Frequently Asked Questions
Are parasitic infections common after organ transplants?
Parasitic infections post-transplant are not common, though the risk depends on the geographic origin of the donor and recipient. Enhanced screening has the potential for early detections, leading to treatments and better outcomes.
What symptoms should I watch out for if I’ve had a transplant?
symptoms like fever, abdominal pain, nausea and vomiting, skin rashes, and any unusual symptoms should be reported to your transplant team promptly. Fast action is critical for triumphant treatment.
Table of Contents