2025-03-01 17:36:00
The Future of Genetic Testing: Targets for Hereditary Cancer Awareness
Table of Contents
- The Future of Genetic Testing: Targets for Hereditary Cancer Awareness
- The Rise of Genetic Awareness
- Understanding BRCA Mutations: What Lies Beneath?
- The Limitations of Current Screening
- Real-World Implications: Conversations and Decisions
- Future Developments in Genetic Testing and Preventative Care
- Community Involvement and Policy Advocacy
- The Journey Toward Better Understanding
- FAQ
- Unlocking Your genetic Code: Understanding BRCA Mutations and Hereditary Cancer Risk – An Expert Interview
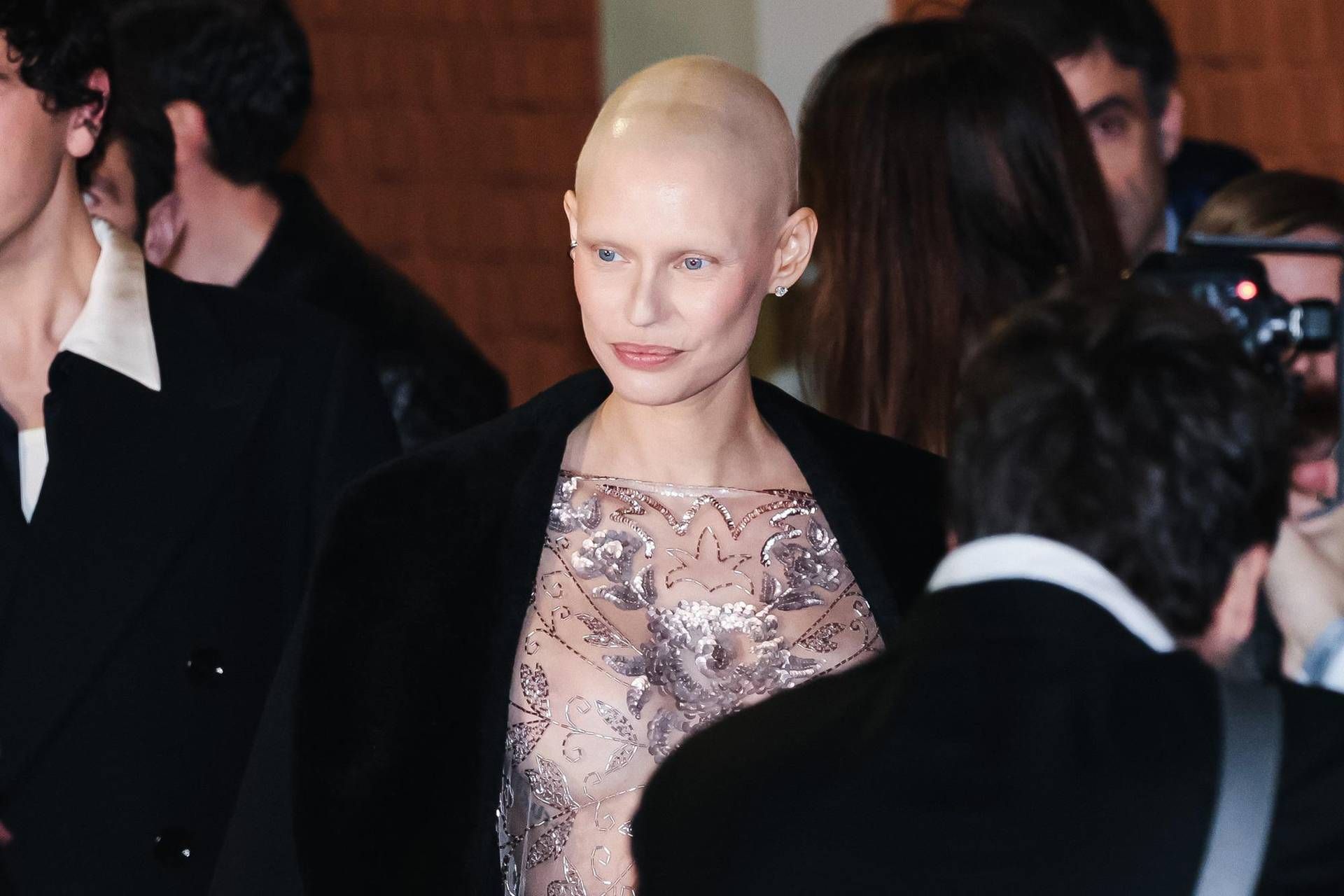
What if knowing your genetic predisposition could empower you to take control of your health? With advancements in genetic testing, particularly concerning inherited mutations such as BRCA1 and BRCA2, the landscape of cancer prevention and treatment is shifting dramatically. In light of recent discussions surrounding public figures like Bianca Balti and the ongoing information campaigns, it is crucial to delve deeper into the implications of these genetic markers and their influence on personal health decisions.
The Rise of Genetic Awareness
As public figures like Bianca Balti bravely share their personal stories about living with hereditary mutations, they illuminate critical topics that may significantly increase awareness and understanding. Indeed, Balti’s candid choices about her health not only highlight her struggles but also serve as a catalyst for broader discussions around cancer awareness. These stories are invaluable; they bridge the gap between clinical knowledge and real-life experiences.
Power of Personal Narratives
Balti’s candid reflections serve as a reminder that life continues despite medical challenges. Her decision not to remove her ovaries or fallopian tubes—even after knowing her predisposition to cancer—resonates with many women who face similar choices. This spotlight on personal narratives can catalyze change at the community level, encouraging others to pursue genetic testing and engage in discussions about hereditary cancer risks.
Campaigns Promoting Genetic Awareness
The information campaign recently launched by AstraZeneca and MSD aims to educate the public about hereditary tumors, urging everyone to be proactive about their health. The slogan “Knowing them is the first step” embodies the essence of this initiative. Through community resources, they aim to demystify genetic testing and encourage individuals to consider their family histories and potential risks.
Understanding BRCA Mutations: What Lies Beneath?
Genetic mutations in BRCA1 and BRCA2 significantly increase a person’s likelihood of developing various cancers, including breast and ovarian cancers. Current research indicates that about 15% of all tumors are related to these mutations, while estimates suggest that up to 20% of high-grade serous ovarian tumors could be hereditary. Despite this, the complexities surrounding genetic predispositions often leave individuals feeling helpless, unsure of their next steps.
The Complexity of Tumor Formation
Oncologist Sunday Lorusso emphasizes that while these mutations do not guarantee tumor formation, they significantly elevate the risk. Such information is vital for women considering genetic testing, highlighting the importance of knowledge and awareness in making informed health decisions. But can this knowledge truly change outcomes?
Primary vs. Secondary Prevention
The challenge, as Dr. Lorusso points out, lies not just in understanding one’s genetic risks but in the prevention strategies that follow. Primary prevention methods, which may include surgical interventions like prophylactic mastectomy or oophorectomy, aim to reduce cancer risk before it manifests. Conversely, secondary prevention focuses on screening to detect cancer early, a critical factor in improving survival rates.
The Limitations of Current Screening
While intriguing, the current screening protocols for ovarian cancer remain limited. Despite recommendations for regular ultrasounds and CA-125 tests, many women still receive late-stage diagnoses due to ovarian cancer’s notoriously subtle beginnings. This reality highlights a significant challenge within the medical community: how to detect ovarian cancer early and effectively.
Understanding Symptoms: The Silent Killer
Historically dubbed a “silent killer,” ovarian cancer often presents with vague symptoms that can be easily mistaken for other gastrointestinal issues. This complexity makes public education increasingly crucial. The responsibility lies not only on healthcare providers but also on advocates and community leaders to raise awareness surrounding these common yet overlooked signs.
The Need for Comprehensive Genetic Testing
Genetic testing protocols have evolved substantially over the years. Initially limited to those with familial histories of early-onset cancers, testing is now being recommended more broadly. Current practices suggest that approximately 30% of mutation-related tumors occur in women without familial risk factors, pressing the need for revised testing approaches and increased public accessibility.
Real-World Implications: Conversations and Decisions
As discussions about genetic testing become more commonplace, the implications of these findings extend beyond individual health decisions. They influence community practices, healthcare policies, and the overall approach to cancer treatment and prevention.
Support Systems and Educational Resources
More than ever, support systems for women facing these challenges are essential. Organizations and advocates should strive to create inclusive spaces for discussion, offering resources that demystify genetic testing and its implications. Engaging individuals in conversations about family planning, lifestyle choices, and regular screenings can lead to improved health outcomes.
Personal Empowerment Through Knowledge
Knowledge is empowering, but it comes with the responsibility to act. Discovering a hereditary predisposition does not equate to an inevitable cancer diagnosis; rather, it opens the door to informed health decisions. Women like Bianca Balti, who share their choices transparently, motivate countless others to seek support and become proactive participants in their health journeys.
Future Developments in Genetic Testing and Preventative Care
As advances in genetic research continue, the future of cancer prevention may take unexpected turns. Innovations in testing methods, screening technologies, and preventative measures promise a more comprehensive approach to hereditary cancers.
Potential Innovations in Detection
Breakthroughs in medical technology may soon yield more reliable methods for early detection of ovarian cancer. These could include liquid biopsies, advanced imaging techniques, or novel biomarkers that facilitate earlier and more accurate diagnoses.
The Role of Artificial Intelligence in Genetic Research
Artificial intelligence may play a pivotal role in analyzing genetic data, offering personalized recommendations based on an individual’s mutation profile. By predicting risks more accurately, AI could enhance preventative strategies, ultimately saving lives. This synergy between technology and genetics may revolutionize how we approach hereditary cancers in the coming years.
Community Involvement and Policy Advocacy
Addressing the complexities of hereditary cancers requires not only scientific advancements but also community involvement and policy advocacy. Raising awareness through campaigns that foster open discussions can contribute to less stigma surrounding genetic tests and facilitate access to necessary resources.
Building a Supportive Ecosystem
Healthcare providers, organizations, and communities must collaborate to build an ecosystem that supports genetic literacy. Workshops, webinars, and community health fairs can provide platforms for discussing hereditary risks and preventive strategies, emphasizing that knowledge is indeed the first step toward prevention.
Overcoming Stigmas and Misunderstandings
Misunderstandings surrounding genetic testing and hereditary risks can foster stigmas that prevent individuals from seeking help. It is essential for society to embrace an open dialogue about these topics, breaking down barriers and dismantling fears associated with genetic testing.
The Journey Toward Better Understanding
Ultimately, the conversation surrounding BRCA mutations and hereditary cancers is an increasingly important one that touches all walks of life. As individuals navigate their family histories and health choices, the engagement of medical professionals, advocates, and society at large will prove vital. By continuing to share stories like Bianca Balti’s and encouraging conversations about the implications of genetic testing, a clearer path toward understanding and prevention can be forged.
FAQ
What are BRCA1 and BRCA2 genes?
BRCA1 and BRCA2 are genes that produce proteins responsible for repairing damaged DNA. Mutations in these genes can lead to an increased risk of certain cancers, particularly breast and ovarian cancer.
How do I know if I should get tested for BRCA mutations?
Discussing your family history with a healthcare provider is crucial. Recommendations may be given for genetic testing if there is a personal or familial history of breast or ovarian cancer.
What are the next steps if I test positive for a BRCA mutation?
If you test positive, working closely with a healthcare team to consider prevention options, such as regular screenings or lifestyle changes, is essential. Discussions about risk-reducing surgeries may also occur.
Unlocking Your genetic Code: Understanding BRCA Mutations and Hereditary Cancer Risk – An Expert Interview
Time.news: Genetic testing for hereditary cancer risk is becoming increasingly prevalent. today, we speak with Dr. Eleanor Vance, a leading genetic counselor [fictional title] specializing in BRCA mutations and cancer prevention, about the future of genetic testing for hereditary cancers. Dr. Vance, thank you for joining us.
Dr. Vance: It’s my pleasure.
time.news: Recent news has focused on public figures like Bianca Balti sharing their experiences.How significant is this increased awareness?
Dr. Vance: It’s incredibly significant.Personal narratives normalize conversations about complex health decisions, especially surrounding BRCA mutations, genetic testing, and options for cancer prevention. When someone in the public eye is open about their journey, it resonates with countless others facing similar choices. It bridges the gap between clinical information and real-world experiences.
Time.news: The article mentions information campaigns, such as the one by AstraZeneca and MSD. What role do these campaigns play in increasing hereditary cancer awareness?
Dr. Vance: These campaigns are vital for dispelling myths and providing accurate information accessibly. The ‘knowing Them Is The First Step’ campaign, for example, really encapsulates the proactive approach we should be encouraging. Genetic testing isn’t something to fear; it’s a tool for empowerment. Campaigns help demystify the process and encourage people to consider their family histories and potential cancer risks.
Time.news: Let’s break down the science. Can you explain, in simple terms, what BRCA1 and BRCA2 genes are and why mutations are so concerning?
Dr.Vance: Think of BRCA1 and BRCA2 genes as your body’s DNA repair crew. They fix damage that naturally occurs in our cells. When those genes have mutations, this repair crew isn’t functioning correctly, leading to an increased risk of certain cancers, especially breast and ovarian cancer. It’s vital to understand a mutation doesn’t guarantee cancer, but it substantially elevates the risk.
Time.news: Our article highlights the challenges of ovarian cancer screening. Why is it so difficult to detect early?
Dr. Vance: Ovarian cancer is often called a “silent killer” because its early symptoms – things like bloating or vague abdominal discomfort – are easily dismissed or attributed to other conditions. Current screening options, such as ultrasounds and CA-125 tests, have limitations, frequently enough detecting cancer only in later stages. This underscores the importance of increased awareness of subtle symptoms and exploring genetic testing, especially with a family history of hereditary cancers.
Time.news: The piece points out a shift towards broader genetic testing recommendations, even without a strong family history. Why this change?
Dr. Vance: We are realizing that a significant percentage of individuals with BRCA mutations, around 30%, have no discernible family history of early-onset cancers. Focusing solely on those with a family history misses a ample portion of at-risk people. Expanding testing criteria allows us to identify individuals previously overlooked, enabling proactive cancer prevention strategies.
Time.news: What are some of those preventive strategies for someone who tests positive for a BRCA mutation?
Dr. Vance: The options are personalized and depend on the individual’s specific mutation, medical history, and personal preferences. They can include more frequent and intensive screening (like mammograms and MRIs for breast cancer), lifestyle modifications, risk-reducing medications, and, in certain specific cases, prophylactic surgery (like mastectomy or oophorectomy) to remove the breasts or ovaries before cancer develops.
Time.news: What advice would you give someone considering genetic testing for hereditary cancer?
Dr. Vance: First, gather your family history. Talk to your relatives about any cancer diagnoses, ages of onset, and types of cancer. Second, discuss your family history with your healthcare provider. They can assess your risk and determine if genetic testing is appropriate. if you proceed with testing, ensure you receive genetic counseling, if needed. Counselors can definitely help you understand the results, implications, and options for managing your risk effectively.
Time.news: The article also mentions potential future advancements, like AI in genetic research and liquid biopsies. What excites you most about the future of hereditary cancer prevention and treatment?
Dr.Vance: The potential of AI to analyze vast amounts of genetic data and provide personalized risk assessments is incredibly exciting. Imagine a world where we can predict an individual’s cancer risk with unprecedented accuracy and tailor preventative strategies accordingly. Liquid biopsies,offering non-invasive early detection,also hold tremendous promise for improving outcomes. These technological advances, coupled with increased awareness and proactive approaches, will transform how we manage hereditary cancers in the years to come.
time.news: Dr. Vance, thank you for your insightful expertise.
dr. Vance: You’re very welcome. Remember, knowledge is power when it comes to your health.