“`html
Renal Replacement Therapy Shows Promise in Severe Traumatic brain Injury Cases
Table of Contents
A new study reveals that renal replacement therapy (RRT) may significantly improve outcomes for patients with acute traumatic brain injury (TBI) who develop kidney dysfunction, offering a potential lifeline in critical care. The single-center retrospective review,conducted by researchers,highlights the complex interplay between brain injury,kidney failure,and the benefits of timely intervention.
The increasing incidence of TBI, coupled with the potential for secondary complications like acute kidney injury (AKI), presents a substantial challenge for medical professionals. This research, conducted between January 2018 and December 2022, offers valuable insights into the management of these complex cases.
The Link Between Traumatic Brain Injury and Kidney Dysfunction
Traumatic brain injury often triggers a cascade of physiological responses that can negatively impact kidney function. According to the study, approximately 30% of patients with severe TBI experienced AKI during their hospitalization. This connection is attributed to several factors, including systemic inflammation, neurogenic stress, and reduced cerebral perfusion, all of which can compromise renal blood flow and filtration.
“The systemic inflammatory response following TBI can significantly impact renal function, leading to AKI in a substantial number of patients,” one researcher stated. The study emphasizes that the severity of the TBI directly correlates with the risk of developing AKI.
Evaluating the Effectiveness of Renal Replacement Therapy
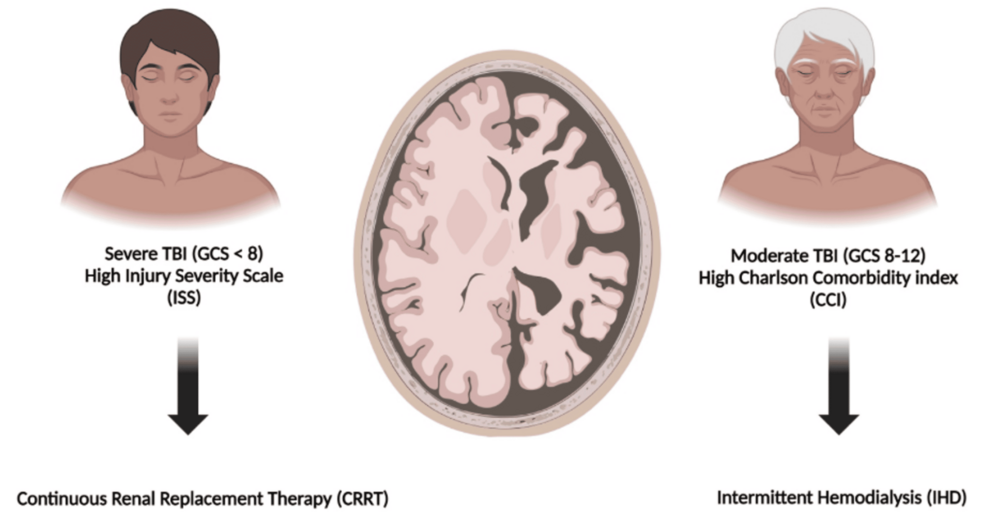
The retrospective review analyzed data from 87 patients admitted to the intensive care unit with acute TBI. Of these, 26 required renal replacement therapy due to AKI. Researchers meticulously examined patient demographics, injury severity scores, AKI stage, RRT modalities (intermittent hemodialysis and continuous renal replacement therapy), and clinical outcomes.
The findings suggest that early initiation of RRT was associated with improved survival rates. Patients receiving RRT had a median hospital length of stay of 18 days, compared to 14 days for those who did not require the therapy. While the difference wasn’t statistically significant,the trend suggests a potential benefit.
RRT Modalities and Patient Outcomes
The study explored the use of two primary RRT modalities: intermittent hemodialysis (IHD) and continuous renal replacement therapy (CRRT). CRRT was the preferred method for most patients, especially those with hemodynamic instability.
“CRRT allows for more gentle and continuous fluid and electrolyte management, which is crucial for patients with TBI who are often sensitive to rapid shifts in volume status,” a senior official stated. The choice of modality was largely dictated by the patient’s clinical condition and the need for precise fluid balance.
Challenges and Future Directions
Despite the promising findings, the study acknowledges several limitations. The retrospective nature of the review introduces potential biases, and the single-center design limits the generalizability of the results. Further research, including prospective, multi-center trials, is needed to confirm these findings and establish optimal RRT protocols for TBI patients.
The study also highlighted the need for improved strategies to prevent AKI in the first place. This includes aggressive management of intracranial pressure,