2025-04-15 07:21:00
The Battle Against Pancreatic Cancer: A New Hope on the Horizon
Table of Contents
- The Battle Against Pancreatic Cancer: A New Hope on the Horizon
- Pancreatic Cancer Breakthrough: Targeting Galectin-1 for New Hope? A Q&A with Cancer Expert, Dr.Anya sharma
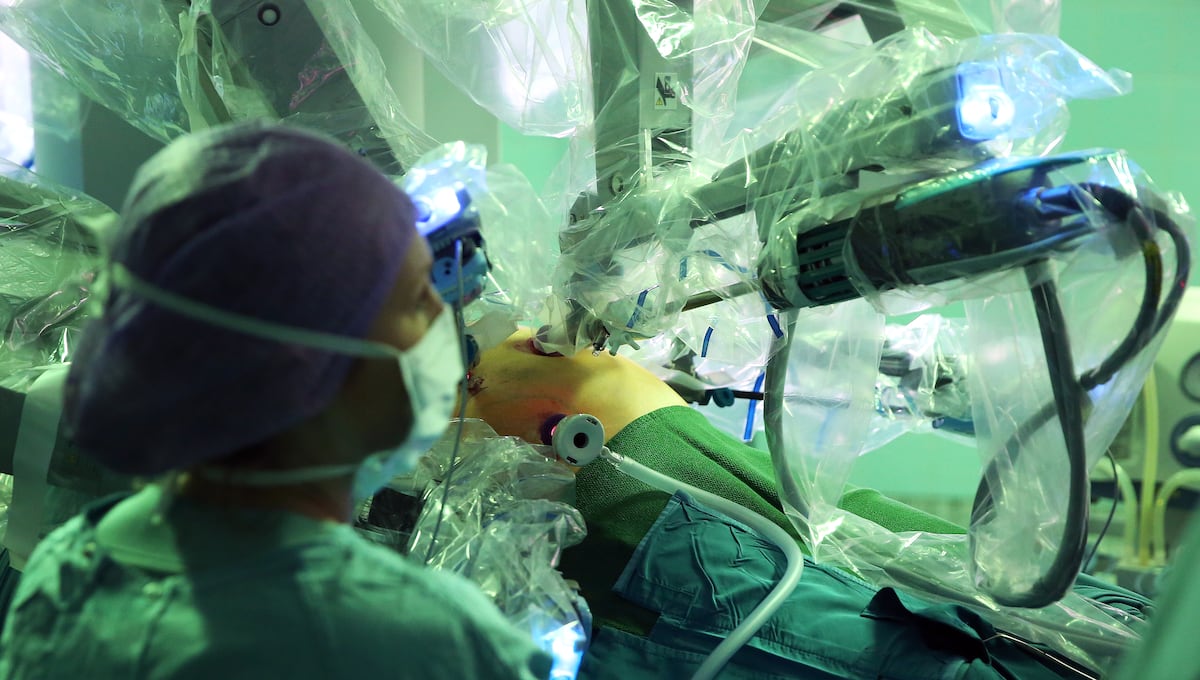
Pancreatic cancer often presents itself as a formidable adversary—one shrouded in mystery and danger. Characterized by its unique ability to construct an impenetrable fortress around its malignant cells, pancreatic tumors remain among the most aggressive of cancers, with a grim survival rate of just over 10% five years post-diagnosis. As researchers grapple with the intricacies of this stubborn disease, recent discoveries are igniting new hope for breakthroughs in treatment strategies. But what does this mean for the future of pancreatic cancer therapy?
Understanding the Tumor Microenvironment
At the heart of pancreatic cancer’s resilience lies the stroma, a dense and fibrous network of cells that engulfs the tumor, creating a protective barrier that impedes effective treatment. This layer is not merely structural; it plays a pivotal role in the tumor’s aggressive nature. Spanish scientists, in a groundbreaking study published in the journal PNAS, have pinpointed a critical mechanism within this stroma that could unlock new therapeutic avenues. Specifically, they have identified a protein called Galectin-1 (Gal1) that seems to play a dual role: it facilitates cancer cell proliferation and shields these cells from the immune system.
The Role of Galectin-1 in Tumor Growth
Pilar Navarro, one of the leading researchers from the Research Institute of the Hospital of the Mar, encapsulates this dynamic succinctly: “If the tumor was a game, the tumor cells are the protagonists and the stroma are the secondary actors.” The discovery that Gal1 is secreted not by the cancer cells themselves but by fibroblasts within the stroma offers invaluable insights. These fibroblasts, when reprogrammed by the cancer, actively support tumor growth by secreting Gal1, which not only prevents immune destruction but also accelerates cancer cell proliferation.
New Functions of Gal1 Revealed
This recent research has unveiled an extraordinary function of Gal1: its presence in the nucleus of fibroblasts alters their identity, transforming them into more aggressive and proliferative cells. The study highlights the intricate relationship between Gal1 and K-Ras, a gene often mutated in 90% of pancreatic cancer cases. When Gal1 levels are high, K-Ras regulation within fibroblasts intensifies, prompting a cycle of relentless growth and aggression. This paradigm shift in our understanding of stroma and tumor interaction opens exciting new doors for targeted therapies.
Exploring Future Therapeutic Strategies
The implications of blocking Gal1 function within the tumor microenvironment are enormous. Navarro posits that while inhibiting the stroma could stall tumor progression, it’s merely one piece of a complex puzzle. “If we inhibit Gal1, we will attack several fronts and can perhaps stop the tumor, but we cannot guarantee complete elimination,” she asserts. This perspective encourages a multifaceted approach to treatment, one that combines therapies targeting different aspects of tumor biology.
A Multi-Targeted Approach in Cancer Treatment
Experts like María José Safont from the Spanish Society of Oncology Medical echo these sentiments, suggesting that the exploration of stromal cells at their core could unveil new therapeutic pathways that enhance treatment efficacy. This could prove especially critical in the American healthcare landscape, where pancreatic cancer continues to manifest as a leading cause of cancer-related mortality. As approximately 10,000 new cases arise each year, incorporating innovation into treatment regimens is crucial.
Innovative Drug Design: The Next Steps
The discovery of Gal1’s multifaceted roles is just the beginning. There’s a keen interest in developing inhibitors that can penetrate cell membranes and target Gal1 within the intracellular environment, a feat not previously imagined. This progression aligns with the ongoing efforts in pharmaceutical research, where understanding molecular dynamics within the tumor microenvironment may lead to the crafting of novel therapeutics.
Integrating Real-World Examples
In the United States, organizations like the Mayo Clinic and various research universities are augmenting these findings with their data. Their investigations explore how stroma manipulation can radically shift treatment landscapes. Notably, the push for integration of multi-targeted therapies mirrors successful strategies in other cancers, such as breast cancer, wherein similar stromal interactions were disrupted to improve patient outcomes.
Collaborating for a Cure
The collaborative nature of recent studies, such as those involving the Mayo Clinic and other research institutions, illustrates the global commitment to combating pancreatic cancer. Not only are researchers in Spain making strides, but medical professionals across the United States are also contributing to understanding and potentially overcoming the disease. Such collaborations pave the way for innovative clinical trials, offering patients hope for new therapies tailored to counteract their specific tumor biology.
Holding the Promise of Change
The future landscape of pancreatic cancer treatment is on the verge of transformation. With Gal1 identified as a crucial player in the growth and sustenance of pancreatic tumors, exploring strategies to inhibit its function could represent a turning point. Moreover, as researchers delve deeper into tumor-stroma interactions, it is becoming increasingly clear that a comprehensive understanding of these relationships will be critical in the development of effective therapies.
Emerging Trends and Technology in Research
As technology advances, the integration of artificial intelligence in drug discovery is fostering rapid advancements in treatment possibilities. AI can analyze vast datasets—identifying potential targets and even predicting how particular clients may respond to therapies based on their unique genetic makeups. Recent studies underscore that the complexities of cancer require not just innovative drug development but also personalized medicine approaches that consider each patient’s unique tumor biology.
FAQ Section
What are the main challenges in treating pancreatic cancer?
The primary challenges in treating pancreatic cancer include its late diagnosis, aggressive nature, and the stroma’s protective barrier that hampers drug efficacy. Current therapies have limited effectiveness, emphasizing the need for new research and innovative treatments.
How does the discovery of Gal1 impact future research?
The identification of Gal1 as a key player in tumor proliferation presents new avenues for research focused on developing inhibitors that target both its extracellular and intracellular functions, potentially enhancing treatment strategies for pancreatic cancer.
What role does the stroma play in pancreatic cancer?
The stroma comprises non-cancerous cells that can be reprogrammed by cancer cells to support tumor growth. This microenvironment acts as a protective barrier and can enhance the aggressiveness of the cancer, complicating treatment efforts.
Pros and Cons of Targeting Gal1
Pros
- May open new avenues for therapeutic development.
- Has potential to enhance the efficacy of current treatment regimens.
- Strengthens the understanding of tumor biology and environment interactions.
Cons
- Inhibition may not guarantee cancer eradication.
- The complexity of the tumor microenvironment may require multi-pronged strategies.
- Potential for unforeseen side effects or resistance mechanisms to emerge.
Staying Engaged: How You Can Help
If you’re passionate about advancements in cancer research, consider supporting organizations dedicated to this cause. Participation in fundraising events, awareness campaigns, and clinical trials can be instrumental in the ongoing fight against pancreatic cancer. The path to a cure requires not only scientific brilliance but also a community of advocates and supporters rallying for change.
For further updates on breakthroughs in oncology, visit our related articles:
- Innovations in Cancer Therapy: Exploring New Frontiers
- Pancreatic Cancer Research: Latest Developments and Future Perspectives
- Understanding Tumor Microenvironments: The Key to Effective Treatment
Stay informed, stay involved, and help champion the future of cancer care!
Pancreatic Cancer Breakthrough: Targeting Galectin-1 for New Hope? A Q&A with Cancer Expert, Dr.Anya sharma
Time.news: Pancreatic cancer remains one of the deadliest cancers, with survival rates stubbornly low. Our recent article highlighted a promising new discovery: the role of Galectin-1 (Gal1) in the tumor microenvironment. Dr.Anya Sharma, a leading expert in oncology and cancer research, joins us too shed light on this development and its potential impact. Dr. Sharma, welcome!
Dr. Anya Sharma: Thank you for having me. It’s crucial to keep the public informed about progress in the fight against pancreatic cancer.
Time.news: Our article focused on how Spanish scientists pinpointed Gal1’s dual role in promoting cancer cell proliferation and shielding them from the immune system within the stroma. Can you elaborate on the significance of this discovery for our readers unfamiliar with the complexities of tumor microenvironments?
dr. Anya Sharma: Absolutely. Think of pancreatic cancer cells as trying to build a fortress. The “stroma” is that fortress, a network of cells surrounding and protecting the cancerous cells.Galectin-1 (Gal1) is like a key construction foreman within that fortress. It’s secreted by fibroblasts, cells within the stroma, and it promotes both the expansion of the tumor (proliferation) and helps it hide from the immune system. The really exciting part is discovering that Gal1 isn’t made by the cancer cells themselves, but manipulated surrounding cells, specifically fibroblasts to produce it. This gives us a new target.
Time.news: The article mentions Pilar Navarro’s analogy of the tumor as a game,with tumor cells as protagonists and the stroma as secondary actors. How does understanding this “supporting cast” change our approach to pancreatic cancer treatment?
Dr. Anya Sharma: Exactly! For years,we’ve focused on directly attacking the “protagonists” – the cancer cells. But this research highlights the crucial role of the “supporting cast” – the stroma. By targeting Gal1 in the stroma, we disrupt the support system the tumor relies upon. This isn’t a magic bullet, but it’s a crucial addition to our arsenal. Imagine trying to siege a fortress – you need to weaken the walls, disrupt supply lines, and target key personnel, not just attack the central tower.
Time.news: The research also uncovered a link between Gal1 and the K-Ras gene, frequently mutated in pancreatic cancer cases. what does that connection tell us about future therapeutic strategies?
Dr. Anya Sharma: That connection is very vital. K-Ras is a notorious oncogene, meaning it drives cancer growth, in many cancers. The finding that Gal1 influences K-Ras activity within fibroblasts suggests that inhibiting Gal1 could possibly dampen down K-Ras-driven growth,not just in cancer cells,but also impacting supportive cells as well. This offers a double whammy.
Time.news: Our article emphasizes the need for a multi-targeted approach. Why is this so critical in pancreatic cancer therapy,and how does targeting Gal1 fit into this broader strategy?
Dr. Anya Sharma: Pancreatic cancer is notoriously complex. The tumor microenvironment is incredibly dense and resilient. So relying on a single drug targeting a single pathway is unlikely to be accomplished. A multi-targeted approach is crucial. Think of it like a coordinated attack on the tumor. Targeting Gal1 is one piece of that strategy, potentially making the tumor more vulnerable to other therapies, like chemotherapy, radiation, or immunotherapy
Time.news: What are some of the challenges in developing drugs that can effectively target Gal1, particularly within the cell?
Dr. Anya Sharma: Getting drugs inside cells is always tricky. Gal1 is an intracellular target inside the fibroblast stroma cell nucleus – that is even more difficult- but that is what makes it such an exciting target. It will need a more precisely targeted medicine. We need drugs that can penetrate cell membranes and selectively inhibit Gal1 without causing widespread toxicity.This requires a new breed of medicines. Fortunately,advancements in drug delivery systems and molecular targeting are making this increasingly feasible.
Time.news: The article highlights the collaboration between research institutions like the Mayo Clinic and those in Spain. How important is this type of international collaboration in accelerating progress in pancreatic cancer research?
Dr.Anya Sharma: Absolutely essential. Sharing data, expertise, and resources among research groups across the globe leads to faster progress and a more comprehensive understanding of the disease. Cancer knows no borders, and neither should our efforts to combat it.collaborative clinical trials are also critical for evaluating new therapies and identifying the most effective treatment strategies.
Time.news: For our readers who want to support advancements in cancer research, what specific steps can they take to make a difference?
Dr. Anya Sharma: there are several ways to get involved. You can support organizations such as the Pancreatic Cancer Action Network (pancan) or the Lustgarten Foundation through donations or participation in fundraising events. Consider volunteering your time to support cancer patients and their families. Learn about clinical trials and consider participating if you meet the eligibility criteria and most importantly, spread the word and raise awareness about the importance of pancreatic cancer research. Early diagnosis and innovative treatments are our best hope for improving outcomes.
Time.news: Dr. Sharma, thank you so much for your valuable insights. This has been incredibly informative.
Dr. Anya Sharma: My pleasure. Let’s continue to shine a light on the fight against pancreatic cancer.