Revolutionizing Dementia Diagnosis: The Breakthrough of the Cortical Asymmetry Index
Table of Contents
- Revolutionizing Dementia Diagnosis: The Breakthrough of the Cortical Asymmetry Index
- The Science Behind the Cortical Asymmetry Index
- Unlocking New Understanding of Dementia Subtypes
- The Technological Leap: Integrating AI in Healthcare
- The Challenges Ahead: Diagnosing Frontotemporal Dementia
- The American Context: Neurodegenerative Diseases at a Glance
- The Path Forward: Fostering Research and Collaboration
- Incorporating Patient Perspectives
- Interactive Elements to Engage and Inform
- Addressing Common Questions Surrounding Dementia
- Conclusion: A New Era in Dementia Management
- Revolutionizing Dementia diagnosis: An interview with dr. Eleanor Vance on the Cortical Asymmetry Index (CAI)
Imagine living in a world where the complexities of neurodegenerative diseases are unraveled, where diagnosis isn’t a guessing game but a precise science. A groundbreaking study led by the clinicians at the Clínic-IDIBAPS in Barcelona is bringing us a step closer to that reality with the introduction of the Cortical Asymmetry Index (CAI). This innovative tool has the potential to redefine how we understand, diagnose, and monitor dementia frontotemporal and Alzheimer’s disease.
This pivotal research has meticulously analyzed neuroimaging from 101 patients with frontotemporal dementia, 230 with Alzheimer’s disease, and 173 healthy individuals, establishing significant patterns that not only discriminate between these conditions but also unveil the specific subtypes of frontotemporal dementia. What if we could harness the understanding gained from this research to create more personalized treatment plans? The possibilities are staggering.
The Science Behind the Cortical Asymmetry Index
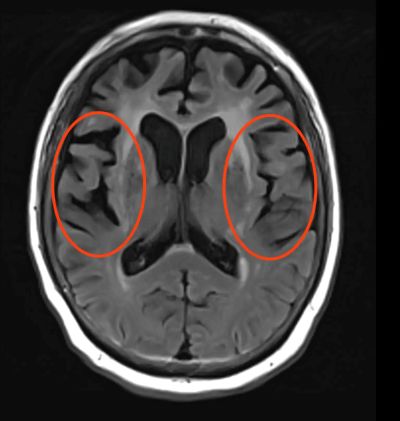
At the core of this pioneering study is the CAI, which quantifies the asymmetry of the brain in patients diagnosed with frontotemporal dementia. The results indicate that an increase in brain asymmetry correlates with the progression of dementia—a discovery that provides an essential window into the disease’s trajectory. This method stands as a superior alternative to traditional qualitative assessments, effectively shifting the diagnostic paradigm in dementia care.
The Methodology
The research team employed magnetic resonance imaging (MRI) to investigate brain structures. By comparing the asymmetrical features of participants’ brains against a control group, they successfully distinguished between those suffering from Alzheimer’s, frontotemporal dementia, and healthy individuals. This methodical approach not only enhances diagnostic accuracy but also addresses a critical gap in the assessment process, especially for frontotemporal dementia, which traditionally lacks reliable biomarkers.
Unlocking New Understanding of Dementia Subtypes
One of the significant advantages of the CAI is its ability to differentiate the subtypes of frontotemporal dementia. Understanding the nuances between the semantic variant—which results in speech deterioration—and the behavioral variant, characterized by personality and conduct alterations, aids in tailoring interventions more effectively. For patients and families grappling with a dementia diagnosis, this nuanced understanding can lead to more targeted therapies and supportive measures.
Follow-Up Findings
Additionally, the research team’s follow-up over two years revealed that higher asymmetry corresponds to not only advanced stages of dementia but also elevated levels of neurofilaments, proteins associated with brain degeneration. This correlation offers clinicians a reliable metric to monitor disease progression and adjust treatment plans dynamically, fostering a proactive approach to managing neurodegenerative diseases.
The Technological Leap: Integrating AI in Healthcare
What truly sets this study apart is the application of artificial intelligence (AI). By incorporating AI algorithms with the CAI, researchers have identified subgroups among dementia patients based on biological differences, further enhancing the understanding of Alzheimer’s and frontotemporal dementia. This marriage of technology and healthcare heralds a new era in medical diagnostics, where AI can analyze patterns and insights previously unnoticed by human eyes.
Open-Sourcing Innovations
The code utilized for the CAI will be available on open-source platforms, inviting researchers worldwide to use and adapt this revolutionary diagnostic tool in their studies. This collaborative approach not only democratizes access to medical advancements but also accelerates research across the globe, pushing the boundaries of what we can achieve in understanding neurodegenerative diseases.
The Challenges Ahead: Diagnosing Frontotemporal Dementia
Despite these advancements, challenges linger. Notably, frontotemporal dementia lacks a reliable diagnostic biomarker, a stark contrast to Alzheimer’s disease. Current diagnostic practices rely heavily on symptom evaluation and qualitative imaging analysis by specialized healthcare providers. As healthcare professionals strive to provide accurate diagnoses, variations in expertise and resources can lead to inconsistent patient outcomes.
The Implications of Misdiagnosis
Misdiagnosis can have profound ramifications for patients and caregivers, altering treatment paths and impacting quality of life. As the CAI gains traction, it promises to mitigate these challenges, offering a standardized assessment method that enhances diagnostic reliability.
The American Context: Neurodegenerative Diseases at a Glance
In the United States, neurodegenerative diseases pose a growing public health challenge. The Alzheimer’s Association reported that over 6 million Americans aged 65 and older are living with Alzheimer’s disease, and that number is projected to rise to nearly 14 million by 2050. By enhancing diagnostic tools like the CAI, we not only improve individual outcomes but also potentially alleviate the broader societal burdens of advanced disease stages.
Case Study: Integrating Innovations in Clinical Practices
Consider a healthcare facility in New York that adopted AI-driven diagnostic tools. By integrating technologies into patient assessments, they observed a notable reduction in misdiagnoses related to frontotemporal dementia, as well as improved patient outcomes through timely interventions. This real-world application showcases the transformative potential of innovations like the CAI when coupled with responsible implementation.
The Path Forward: Fostering Research and Collaboration
Looking ahead, the key to further advancements lies in collaboration between researchers, healthcare providers, and technological experts. For instance, improving access to neurological imaging technology can enhance the integration of tools like CAI in various clinical settings across the U.S. Moreover, funding for research into neurodegenerative diseases can fuel the development and refinement of diagnostic indices.
Future Research Areas
Potential research avenues include examining the genetic factors contributing to the variations in asymmetry observed in patients and evaluating the long-term effectiveness of CAI in clinical practice. Furthermore, longitudinal studies are essential to validate the findings of this initial research and expand upon the understanding of the indices impacting dementia and neurodegeneration overall.
Incorporating Patient Perspectives
It is crucial to also incorporate patient perspectives into future research and development efforts. Engaging with patients and caregivers provides invaluable insights into the lived experiences of those affected by dementia, enabling researchers to hone their tools and practices to be more patient-centric.
Advocacy and Support Systems
As we push towards enhanced diagnostic tools, advocacy groups and support systems play a pivotal role in guiding families through the diagnosis process, ensuring that patients receive timely and appropriate care. These networks can work hand-in-hand with clinicians to provide a holistic approach to patient wellbeing.
Interactive Elements to Engage and Inform
As we delve deeper into the world of dementia research, consider engaging with channels that keep you informed. For instance, would you like interactive poll features embedded within articles that gauge reader understanding of dementia diagnoses? Such elements can foster a community of informed readers passionate about neurodegenerative disease awareness.
Quick Facts About Dementia
- Frontotemporal dementia is the second most common form of dementia in individuals under 65.
- Current diagnosis often depends on subjective evaluations rather than objective biomarkers.
- Neuroimaging advancements are paving the way for more accurate diagnostic tools.
Addressing Common Questions Surrounding Dementia
What is frontotemporal dementia?
Frontotemporal dementia represents a group of neurodegenerative disorders that primarily affect the frontal and temporal lobes of the brain, resulting in marked changes in personality, behavior, and language abilities.
How does the CAI improve diagnosis?
The CAI provides a quantitative assessment of brain asymmetry, allowing for more accurate differentiation between dementia types and stages, thus enhancing the overall diagnostic process.
What are the implications of these findings for patients?
By utilizing CAI, clinicians may offer personalized treatment plans and better monitor disease progression, ultimately leading to improved patient outcomes and support.
Conclusion: A New Era in Dementia Management
The unveiling of the Cortical Asymmetry Index by the research team at Clínic-IDIBAPS marks a monumental shift in how we understand and diagnose dementia. As we continue to integrate technology with healthcare, we foster a future where accurate diagnosis and personalized treatment become the norm rather than the exception. The promise of new tools like the CAI is not just a triumph of science; it’s a beacon of hope for millions navigating the challenges of dementia.
Engage with us—what are your thoughts or experiences with dementia diagnostics? Your voice matters in this conversation, and together, we can drive awareness and progress in this vital field.
Revolutionizing Dementia diagnosis: An interview with dr. Eleanor Vance on the Cortical Asymmetry Index (CAI)
Time.news Editor: Dr. Vance, thank you for joining us. The recent advances surrounding the Cortical Asymmetry Index (CAI) are generating a lot of buzz. For our readers who are unfamiliar, can you briefly explain what the CAI is and why it’s considered a breakthrough in dementia diagnosis?
dr. eleanor Vance: certainly.The Cortical Asymmetry Index, or CAI, is a new method developed by researchers at Clínic-IDIBAPS in Barcelona too quantify the asymmetry of the brain using MRI scans. It’s particularly helpful in differentiating between Alzheimer’s disease, frontotemporal dementia (FTD) and even distinguishing between subtypes of FTD [According to the provided article]. this is a breakthrough because, unlike Alzheimer’s, FTD has lacked reliable biomarkers, making diagnosis challenging.
Time.news Editor: So, the CAI helps address a crucial diagnostic gap. what specific challenge in diagnosing frontotemporal dementia does the CAI overcome?
Dr. Vance: Currently, diagnosing FTD relies heavily on symptom evaluation and qualitative imaging analysis conducted by specialists.This process can be subjective,leading to potential misdiagnoses [According to the provided article]. The CAI introduces a standardized, quantitative assessment, offering a more objective and reliable approach to identify the disease and its subtypes. This is crucial because misdiagnosis can lead to inappropriate treatment plans and negatively impact the patient’s quality of life.
Time.news Editor: the study highlights the use of artificial intelligence (AI) in conjunction with the CAI. How does AI contribute to the effectiveness of this diagnostic tool for neurodegenerative diseases?
Dr. Vance: AI algorithms can analyze complex patterns in neuroimaging data that might be missed by the human eye. In the context of the CAI, AI helps identify subgroups within dementia patients based on subtle biological differences [According to the provided article], providing a more nuanced understanding of both Alzheimer’s and frontotemporal dementia. This deeper understanding can lead to more targeted and personalized treatment strategies. The integration of AI truly represents a leap forward in medical diagnostics and specifically dementia care.
Time.news Editor: The research team plans to make the CAI code open-source. What impact do you anticipate this will have on the field of neurodegenerative disease research?
Dr. Vance: Open-sourcing the CAI code is a game-changer. It democratizes access to this advanced diagnostic tool [According to the provided article], allowing researchers worldwide to utilize and adapt it for their studies. This collaborative approach will undoubtedly accelerate research efforts,foster innovation,and push the boundaries of our understanding of neurodegenerative diseases. It will also empower smaller research teams or those in resource-limited settings to contribute meaningfully to the field.
Time.news Editor: The article also touches upon the growing prevalence of neurodegenerative diseases in the United States. how can tools like the CAI help alleviate the societal burden associated with these conditions?
Dr. Vance: Early and accurate diagnosis is paramount in managing neurodegenerative diseases effectively. By improving diagnostic accuracy, the CAI can lead to timely interventions, allowing patients to receive the appropriate care and support sooner [According to the provided article]. This not only improves individual outcomes but also perhaps delays disease progression, reducing the need for more intensive and costly care in the later stages. Moreover, accurate diagnoses help families better prepare for the challenges ahead, both emotionally and practically.
Time.news Editor: For our readers who are concerned about dementia, particularly frontotemporal dementia, what practical advice can you offer based on these findings?
Dr. vance: Firstly, it’s crucial to be aware of the signs and symptoms of FTD, which can include changes in personality, behavior, and language abilities [According to the provided article]. If you or a loved one experiences these symptoms, seek evaluation from a qualified neurologist or geriatrician. Secondly, remember that research is constantly evolving, and new diagnostic tools like the CAI are becoming available. Don’t hesitate to ask your healthcare provider about the latest advancements in dementia diagnosis and treatment. connect with advocacy groups and support systems for guidance and resources.
Time.news Editor: What are the next steps in research and development for the CAI, and what future applications do you envision for this technology?
Dr. Vance: Future research will likely focus on validating the CAI’s effectiveness in larger and more diverse populations.Longitudinal studies are needed to assess its long-term impact on patient outcomes and monitor disease progression. Additionally,exploring the genetic factors contributing to brain asymmetry could reveal new insights into the underlying mechanisms of dementia.I envision the CAI becoming an integral part of the routine diagnostic workup for dementia, facilitating earlier and more accurate diagnoses, and ultimately, leading to more effective and personalized treatments. Moreover, there are researchers looking into blood tests for Alzheimer’s disease, and it’s possible that CAI could work in conjunction with those tests, improving diagnostic accuracy for a larger patient population [[3]].
Time.news editor: Dr. Vance, thank you for sharing your insights with us today. This has been incredibly informative and offers a hopeful outlook for the future of dementia diagnosis and management.

